In some patients with cancer, tumors don’t shrink in response to chemotherapy and these patients are more likely to develop metastatic cancer. Mouse studies have shown that for some drug-resistant cancers, chemotherapy can actually promote metastasis. Now, a study published on December 31 in Nature Cell Biology links the spread of breast cancer from resistant tumors in mice to extracellular vesicles these cancer cells secrete and shows an uptick in their potential to cause metastasis after treatment with some chemotherapeutic drugs.
“We were surprised to see that chemotherapy was enhancing this process of metastasis, mediated by the vesicles,” says Michele De Palma, a cancer biologist at the École Polytechnique Fédérale de Lausanne and one of the paper’s authors. “This was quite counterintuitive.”
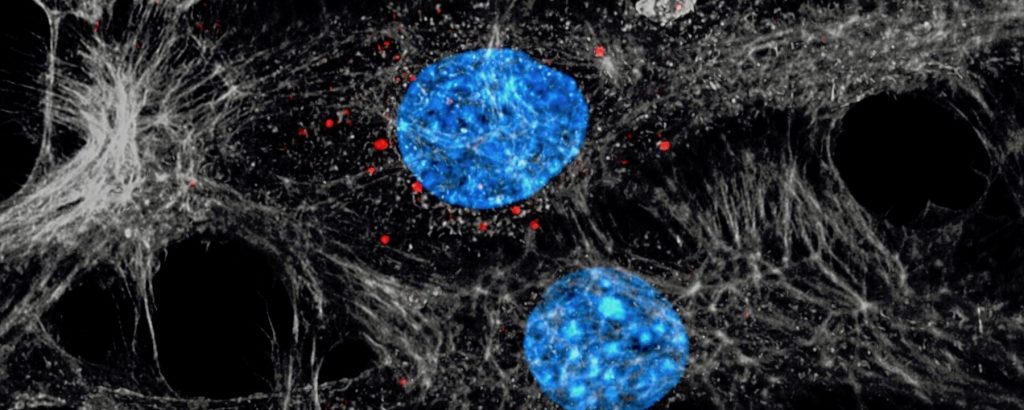
Many types of cells produce extracellular vesicles, known as exosomes when they’re a particular size, packages of biomolecules that are sent to other destinations in the body. For cancer, researchers suspect they are involved in seeding new malignancies far away from the original tumor. “They carry tumor material protected by a membrane and they can travel very long distances in the body and maybe have an effect at a distant location,” says Mikael Pittet, a cancer immunologist at Massachusetts General Hospital and Harvard Medical School, who was not involved with the work.
See “Extracting Exosomes to Detect Signs of Cancer in Urine”
Previous studies have linked exosomes from tumor cells to metastasis in mice. But in this work, the researchers wondered whether chemotherapy could change exosome secretion or contents, with knock-on consequences for their potential to cause metastasis.
The study examined drug-resistant tumors. “We wanted to focus on a condition that you see in patients, not so rarely, because a good fraction of the patients are resistant,” says De Palma.
He and his colleagues gave two commonly used neoadjuvant chemotherapeutics, drugs used to shrink tumors before surgical removal, for breast cancer, paclitaxel and doxorubicin, to mice with chemo-resistant mammary tumors that serve as a model for this condition in humans. They observed that the mice’s tumors metastasized and secreted more exosomes than those from animals with chemo-resistant cancer that weren’t treated.
The scientists isolated the exosomes from chemo-treated tumors and found that they were loaded with a group of proteins called annexin A6, compared to exosomes from untreated tumors. These exosomes were labeled with a fluorescent protein so that researchers could watch where they went in the body. They saw that the exosomes made their made their way to the endothelial cells of the lungs, where breast cancer often spreads.
“They found that these vesicles were actually different when mice were treated with these drugs. Not only were they different, but they were different in a way that suggested that these vesicles could do more harm than without the treatment,” says Pittet.
When the investigators injected exosomes from chemo-treated tumors along with cancer cells into mice that didn’t originally have tumors, they observed that the exosomes induced metastasis.
To test the importance of the annexin A6 proteins another way, the scientists used cancer cells tweaked so they still secreted exosomes, but without annexins. When these exosomes were injected with cancer cells into other mice, the recipient animals produced fewer metastatic deposits in the lung.
Homing in on the lung tissue, the researchers found that the exosomes likely help direct circulating tumor cells shed from the primary breast tumor to the lung through another protein that lures in inflammatory cells called monocytes. “These are bad cells,” De Palma explains. “Monocytes actually help these circulating cancer cells to find a way to form metastasis in the lung.” When the researchers engineered a mouse model so it couldn’t produce this type of monocyte, they again saw that metastasis did not increase.
The different experiments connect the dots in a way that could explain how chemotherapy promotes some resistant breast cancers to spread. The proposed mechanism is that the drug prompts resistant tumors to package up annexin A6 proteins into exosomes that are shipped out in the bloodstream. The exosomes deliver their cargo to the lungs and bad actor monocytes help seed new tumors.
After all this work in mice, the researchers looked at the blood of patients receiving these same neoadjuvant drugs to treat breast cancer. Here again they saw a bump in the annexin A6 proteins present in vesicles of most of the patients relative to before receiving chemotherapy. However, because of the small sample size of six patients, “it does not say anything about whether annexin is pro-metastatic in patients. We just know that it is there,” says De Palma.
“It’s very interesting data even if it’s preliminary,” says Mikala Egeblad, a cancer biologist at Cold Spring Harbor Laboratory who was not part of this research. “One can use the findings that there’s release of these extracellular vesicles to think about biomarkers to predict who may or may not respond to neoadjuvent chemotherapy,” she says.
Future work could show whether these findings are actually relevant for people, but it would require following patients for a long time because breast cancer metastasis can be delayed by 10 years or more, De Palma says.
“Our paper doesn’t say chemotherapy is bad, that chemotherapy is dangerous,” says De Palma. Instead, it investigates the mechanisms by which tumors can adapt. The many patients currently receiving chemotherapy shouldn’t be alarmed, as these drugs’ benefits still outweigh potential negative side effects, De Palma tells The Scientist.
See “How Cancers Evolve Drug Resistance”
In fact, this work offers several paths to pursue to improve the treatment of patients, such as blocking monocytes or one of the proteins involved in this process, says cell biologist and oncologist David Lyden at Weill Cornell Medical College. “Maybe this is the best therapy, but there’s always ways of improvement.”