Studies in mice have shown how low-grade blood infections by the common yeast Candida albicans can trigger inflammatory responses in the brain that temporarily affect memory, but also trigger the formation of granuloma-type structures that share features with the plaques that are found in Alzheimer’s disease (AD).
Led by a Baylor College of Medicine team, the researchers say their results should support future studies on the longer-term neurological consequences of fungal infections in the brain, especially in light of prior research suggesting that fungal infections that cause airway allergic diseases and sepsis are associated with an increased risk for the later development of dementia.
“These findings suggest that the role fungi play in human illness potentially goes well beyond allergic airway disease or sepsis,” commented David B. Corry, PhD, professor of medicine-immunology, allergy, and rheumatology and Fulbright Endowed Chair in Pathology at Baylor College of Medicine. “The results prompted us to consider the possibility that in some cases, fungi also could be involved in the development of chronic neurodegenerative disorders, such as Alzheimer’s, Parkinson’s and multiple sclerosis. We are currently exploring this possibility.”
Corry’s team reported the findings from their latest mouse studies in Nature Communications, in a paper titled, “Microglia and amyloid precursor protein coordinate control of transient Candida cerebritis with memory deficits.”
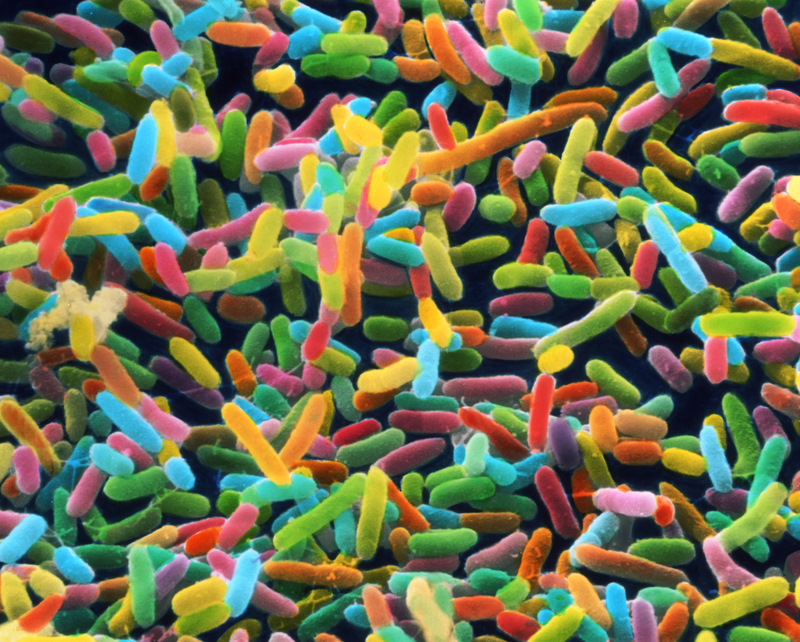
Environmental fungi are increasingly being recognized as either causing or contributing to a wide range of common chronic, cutaneous, and mucosal inflammatory conditions, ranging from eczema to asthma and colitis. Fungi also now represent a major cause of more invasive diseases such as sepsis, especially in hospital settings. “Bloodborne infections with Candida albicans are an increasingly recognized complication of modern medicine,” the authors added.
Candidema and fully invasive candidiasis caused primarily by C. albicans and related species has emerged as one of the leading causes of bloodstream infections in nosocomial settings in developed countries, causing high mortality and costing more than $1 billion annually in the U.S., the authors explained. Diagnosing candidemia can be difficult, which means a better understanding of all fungal disease pathogenesis, diagnosis, and treatment has now become “an essential medical challenge of the 21st century.”
“An increasing number of clinical observations by us and other groups indicates that fungi are becoming a more common cause of upper airway allergic diseases such as asthma, as well as other conditions such as sepsis, a potentially life-threatening disease caused by the body’s response to an infection,” noted Corry, who also is a member of the Dan L. Duncan Comprehensive Cancer Center. Importantly, he pointed out, fungal infections causing airway allergic diseases and sepsis have been associated with increased risk for dementia. “Fungi are further implicated in diseases as diverse as rheumatoid arthritis and Alzheimer’s disease,” the authors wrote.
High-grade candidemia a rapidly lethal to humans and mice, but candidemia in humans will most often be low-grade. As the authors pointed out, short-term fungal infections are recognized as an increasingly common medical problem, but the long-term health effects of transient candidemia aren’t well understood. Corry’s team generated a mouse model to investigate the effects of transient candidemia and Candida cerebritis on the brain, and to try to better understand cerebral immune mechanisms that act to clear such infections.
They injected a single dose of 25000 C. albicans yeast cells directly into the bloodstream of young, healthy experimental mice. The infection was tolerated well, and didn’t result in any major abnormalities either over the short or long term. What the researchers were surprised to find, however, was that the C. albicans yeast cells readily crossed the blood-brain barrier (BBB). “The CNS is uniquely protected from toxic and microbial challenges by the BBB, hence it is surprising that hematogenously acquired C. albicans could readily pass the BBB to proliferate in the brain parenchyma of our mice,” the team wrote. “We thought that yeast would not enter the brain, but it does,” Corry stated.
Tests showed that the yeast caused localized cerebritis in the infected animals, which triggered activation of resident microglial cells. The activated microglial and astroglial cells accumulated around clumps of yeast cells to form unique granuloma structures that also contained amyloid precursor protein within the granuloma periphery, and cleaved amyloid beta peptides that surrounding the yeast cells themselves. These amyloid molecules are typically found in plaques that are characteristic of Alzheimer’s disease.
“In the brain, the yeast triggered the activity of microglia, a resident type of immune cell,” Corry continued. “The cells became very active ‘eating and digesting’ the yeast. They also produced a number of molecules that mediated an inflammatory response leading to the capture of the yeasts inside a granule-type structure inside the brain. We called it fungus-induced glial granuloma, or FIGG.”
Interestingly, the yeast-infected mice also developed temporary spatial memory problems, but these disappeared when the animals immune responses naturally cleared the infections, which took about 10 days. “Our mice further developed memory deficits, another hallmark of AD, albeit a transient form that resolved with fungal clearance,” the team pointed out. However, even after the infection had been cleared the microglia remained active, and the FIGGs persisted for at least three weeks from initial infection.
“Regardless of any possible link to AD, we have shown that transient fungemia in healthy mice has important physiological consequences, including alterations in working memory,” the authors concluded. They suggested that while individual episodes of fungal infection will most commonly be transient, it is conceivable that the effects of repeated low-grade infections over many years could eventually lead to permanent brain damage and long-term cognitive problems. “Thus, although a single low-grade challenge with C. albicans is quickly resolved and results in only transient physiologic derangement as shown here, the broader concern with chronic fungemia is diffuse end-organ injury, which in the CNS [central nervous system] could include substantial neuronal loss and long-term, progressive cognitive impairment … our findings suggest that resolution of low-grade CNS fungal infections through the use of antifungals and other means might preclude or even reverse attendant cognitive decline.”
Corry suggested that greater insights into how fungal infections develop and are cleared will also help scientists develop new antifungal treatment strategies, “… if we better understand how our immune system deals with this kind of constant threat and what are the weaknesses in our immunological armor that occur with aging that allow fungal disease to take root, then we would likely increase the possibility of finding ways to fight back.”