Abstract
Fetal exposure to gestational diabetes mellitus (GDM) predisposes children to future health complications including type-2 diabetes mellitus, hypertension, and cardiovascular disease. A key mechanism by which these complications occur is through stress-induced dysfunction of endothelial progenitor cells (EPCs), including endothelial colony-forming cells (ECFCs). Although several approaches have been previously explored to restore endothelial function, their widespread adoption remains tampered by systemic side effects of adjuvant drugs and unintended immune response of gene therapies. Here, we report a strategy to rejuvenate circulating vascular progenitor cells by conjugation of drug-loaded liposomal nanoparticles directly to the surface of GDM-exposed ECFCs (GDM-ECFCs). Bioactive nanoparticles can be robustly conjugated to the surface of ECFCs without altering cell viability and key progenitor phenotypes. Moreover, controlled delivery of therapeutic drugs to GDM-ECFCs is able to normalize transgelin (TAGLN) expression and improve cell migration, which is a critical key step in establishing functional vascular networks. More importantly, sustained pseudo-autocrine stimulation with bioactive nanoparticles is able to improve in vitro and in vivo vasculogenesis of GDM-ECFCs. Collectively, these findings highlight a simple, yet promising strategy to rejuvenate GDM-ECFCs and improve their therapeutic potential. Promising results from this study warrant future investigations on the prospect of the proposed strategy to improve dysfunctional vascular progenitor cells in the context of other chronic diseases, which has broad implications for addressing various cardiovascular complications, as well as advancing tissue repair and regenerative medicine.
Introduction
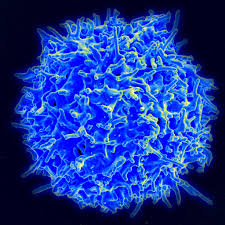
Cardiovascular disease is the most prevalent cause of mortality and morbidity among patients with diabetes1. Adults with diabetes have a two to six times higher risk of developing cardiovascular disease than unaffected individuals2. Similarly, fetal exposure to gestational diabetes mellitus (GDM), which affects 6–15% of all pregnancy, predisposes children to future health complications including type 2 diabetes mellitus (T2DM), hypertension, and cardiovascular disease3,4,5. Although the pathophysiology that links diabetes and cardiovascular disease is complex and multifactorial, there is a general agreement that hyperglycemia and oxidative stress lead to stress-induced early endothelial dysfunction6, which is responsible for both macrovascular (i.e., peripheral artery disease, stroke) and microvascular (i.e., diabetic nephropathy, retinopathy) complications7,8,9. Several pre-clinical and clinical trials are exploring the therapeutic effect of stem and progenitor cell therapies to repair the damaged endothelium and promote neovascularization10,11,12. One promising autologous cell source is endothelial colony-forming cells (ECFCs), a subtype of endothelial progenitor cells (EPCs), identified from circulating adult blood and highly enriched in human umbilical cord blood13,14. As putative EPCs, these ECFCs express robust proliferative potential in forming secondary and tertiary colonies, as well as de novo blood vessel formation in vivo13. Nonetheless, hyperglycemia and a diabetic intrauterine environment also cause premature senescence and significant dysfunction of ECFCs, which limit their therapeutic use3,15,16. ECFCs isolated from patients with diabetes demonstrate delayed colony formation, reduced cell migration, and impaired vasculogenic potential3,15,17. Therefore, restoring dysfunctional ECFCs could improve their vasculogenic potential and serve as biomarkers to assess cardiovascular disease risk10,11.
Several approaches have been explored to rejuvenate ECFCs and to restore their therapeutic potential. These approaches include the delivery of adjuvant drugs to improve immobilization of progenitor cells, genetic modification of cells to overexpress growth factors, and pre-conditioning of these cells with pharmacological agents18,19,20,21. Nonetheless, adjuvant agents need to be maintained at high and sustained systemic levels for efficacy, while genetically modified cells pose high regulatory and cost barriers, which altogether hinder their clinical implementation22. Efforts to enhance the stability and effective presentation of bioactive molecules for improving the therapeutic potential of ECFCs have included attempts to judiciously conjugate vascular endothelial growth factor (VEGF) onto the surface of microparticles23, as well as presentation of proteins and glycomimetic agents to the cell surface17,18,24,25. Despite recent progress in these areas26, translational challenges persist for rejuvenating EPCs using growth factor and gene therapies, including unintended immune response, enzymatic degradation, and uncertain toxicology 27,28,29.
We report a class of liposomal nanoparticles with tunable release kinetics, which can be conjugated directly onto the cell surface to improve the therapeutic potential of ECFCs isolated from infants born to women with gestational diabetes mellitus (GDM-ECFCs). This work builds on the discovery that GDM-ECFCs have decreased vasculogenic potential and altered gene expression, particularly transgelin (TAGLN)3,30, also known as smooth muscle protein 22α (SM22α). We previously reported that increased TAGLN expression in GDM-ECFCs is associated with disrupted actin cytoskeletal rearrangement, which results in reduced cell migration and impaired vasculogenesis3,30,31. Since TAGLN is a direct target of the TGF-β/Smad3 pathway32, we hypothesized that delivering TGF-β inhibitor (SB-431542) directly to the surface of the cells could normalize TAGLN expression and eventually improve cell migration, which is a critical key step in establishing functional vascular networks. Liposomal formulation of nanoparticles was selected for the fabrication technique because it can form multilamellar structures with high encapsulation efficiency and exhibits controllable release kinetics33,34. Moreover, since a similar formulation of liposomal nanoparticles has been previously used to deliver adjuvant drugs to hematopoietic stem and progenitor cells (HSPCs) without adverse immune response22,35, the utilization of liposomal nanoparticles can ease the clinical translation of our strategy 36.
We demonstrate that such lipid-based nanoparticles can robustly bind onto the surface of GDM-ECFCs without altering cell viability and key ECFC phenotypes. More importantly, bioactive nanoparticles can significantly normalize TAGLN expression, restore cell migration, as well as improve vasculogenesis in vitro and in vivo. Collectively, with localized and sustained pseudo-autocrine stimulation of therapeutic cells with bioactive nanoparticles, we present a potentially promising strategy to rejuvenate GDM-ECFCs and improve their therapeutic potential to regenerate the vasculature and address a range of cardiovascular complications that precipitate from GDM.
Results
Engineering bioactive nanoparticles to the cell surfaces
Based on our previous findings that TAGLN inhibition can enhance the functionality of GDM-ECFCs15,30, we designed a nanocarrier system to deliver small molecule SB-431542 (TGF-β inhibitor) for sustained pseudo-autocrine stimulation to therapeutic cells (Fig. 1a). Utilizing a lipid formulation that includes thiol-reactive maleimide headgroups35, multilamellar lipid nanoparticles with a desired size of 150 nm in diameter were engineered to control the release of bioactive agents (Fig. 1b and Supplementary Fig. 1). The targeted size and multilamellar structures of the nanoparticles were chosen because previous studies with these similar parameters showed high encapsulation efficiencies and minimal inflammatory responses following in vivo implantation35. Using Dynamic Light Scattering (DLS) and Nanosight measurements, we confirmed that the multilamellar lipid nanoparticles with 147 ± 63 nm diameter were stable for at least 30 days at both 4 °C and 37 °C (Fig. 1c, d and Supplementary Fig. 2), which is suitable for long-term storage and clinical applications. To stably couple bioactive nanoparticles to the surface of ECFCs, we exploited the high level of reduced thiol groups present on the surface of many progenitor cells37,38. First, we detected substantial amounts of free thiols on ECFCs (Supplementary Table 1). Despite some variations between biological replicates from different patient samples, there were no significant differences between the level of free thiols among normal ECFCs and GDM-ECFCs (p > 0.688; Supplementary Fig. 3). Next, nanoparticles were conjugated to the surfaces of ECFCs using a benign maleimide-thiol coupling, followed by in situ PEGylation to quench residual reactive groups of the nanoparticles (Fig. 1a)38. Upon conjugation, the nanoparticles were successfully attached to the cell surfaces (Fig. 1e). Increasing the ratio of cells to nanoparticles from 1:100 to 1:5,000 correlates well with the increase in the mean fluorescence intensity (MFI) as detected by flow cytometry analysis (Fig. 1f). Since the MFI from samples with cells to nanoparticles ratio of 1:5,000 starts to deviate from linearity, we determined that 5,000 (±100) was the maximum number of particles that can be conjugated on the surface of ECFCs without affecting cell viability and proliferation (Fig. 1f, g and Supplementary Fig. 4). These findings are consistent with previous studies reporting that attachment of nanoparticles, each 150 nm in diameter, would occlude only 5% of the surface of a typical 20-μm-diameter cell35,38. Moreover, nanoparticles could be loaded with various concentrations of the hydrophobic small molecule (SB-431542) and demonstrated consistent week-long drug release profiles (Fig. 1h). By fitting the drug release kinetic to the Korsmeyer-Peppas model39, n values of 0.52 to 0.63 were obtained, suggesting that non-Fickian diffusion is the main driving force of drug release (Fig. 1h and Supplementary Fig. 4). Based on these findings and previous studies that reported a lack of an inflammatory response from innate immune cells exposed to the nanoparticles35,38, we utilized these lipid multilamellar nanoparticles (up to 1:5,000 ratio) loaded with 40 µM SB-431542 for our subsequent in vitro functionality and in vivo therapeutic studies.