Abstract
Colistin remains one of the last-resort therapies for combating infections caused by multidrug-resistant (MDR) Enterobacterales, despite its adverse nephro- and neuro-toxic effects. This study elucidates the mechanism of action of a non-antibiotic 4-anilinoquinazoline-based compound that synergistically enhances the effectiveness of colistin against Salmonella enterica. The quinazoline sensitizes Salmonella by deactivating intrinsic, mutational, and transferable resistance mechanisms that enable Salmonella to counteract the antibiotic impact colistin, together with an induced disruption to the electrochemical balance of the bacterial membrane. The attenuation of colistin resistance via the combined treatment approach also proves efficacious against E. coli, Klebsiella, and Acinetobacter strains. The dual therapy reduces the mortality of Galleria mellonella larvae undergoing a systemic Salmonella infection when compared to individual drug treatments. Overall, our findings unveil the potential of the quinazoline-colistin combined therapy as an innovative strategy against MDR bacteria.
Introduction
Antibiotic resistance is one of the most important threats to human health worldwide and it is concomitant with the urgency of developing new effective antimicrobial compounds. The acquisition of antibiotic resistance mechanisms by bacteria has been attributed to the selective pressure imposed by environmental, human and animal healthcare, general overuse and misuse of these compounds, and to the scarcity in drug development by the pharmaceutical industry1,2.
Bacterial infections are commonly treated with bacteriostatic or bactericidal drugs. Although very effective, alternatives, such as the development of anti-virulence agents that block key pathogenesis mechanisms (pathoblockers), are promising strategies to diminish the emergence of antibiotic resistance mechanisms3. In addition, alternative new drugs can act as adjuvants and reduce the effective concentration of commonly used antibiotics and minimize the emergence of resistance.
In this context, the WHO has classified Salmonella as a high-priority group for the development of new antibacterial therapies4,5. Salmonella senses environmental changes and responds to the detection of host cues by triggering a virulence program. PhoP/PhoQ is a signal transduction cascade that belongs to the bacterial family of two-component regulatory systems (TCS) and has an essential role during the infection of Salmonella into the mammalian host. This TCS consists of PhoQ, a transmembrane sensor with bifunctional histidine kinase/phosphatase activity, and PhoP, a cytoplasmic response regulator6. The system responds to input signals that bacteria encounter during their life cycle, such as availability of Mg2+, presence of long chain unsaturated fatty acids or cationic antimicrobial peptides (CAMPs) and acidic pH7,8,9 As adaptive output responses, PhoP/PhoQ controls the expression of genes involved in magnesium homeostasis10,11, LPS-modifications12, resistance to acidic pH13 the internalization and survival within either phagocytic or non-phagocytic cells14.
The PhoP/PhoQ system has a crucial role during the life cycle of Salmonella and the absence of TCS in mammals, make this TCS an optimal target to develop new antimicrobial therapies15. In this regard, we have recently identified two quinazoline-based compounds which negatively regulate PhoP-activated genes by targeting the PhoQ histidine-kinase activity16.
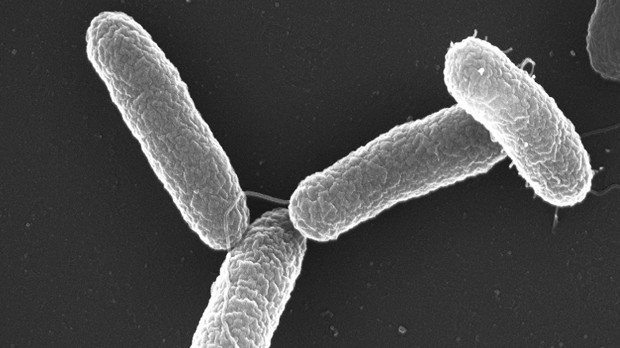
Colistin is a member of the polymyxins that are cationic antimicrobial oligopeptides composed of a cyclic heptapeptide linked to a tripeptide acylated at its N-terminus by a fatty acid17. These antibiotics disorganize the bacterial envelope in two stages: (1) they interact electrostatically with the negative charges of lipid A, displacing Ca2+ and Mg2+ that stabilize LPS, and (2) the acylated chain inserts within the outer membrane (OM) with formation of pores, promoting the own entry of the molecule into the periplasm. Then, the antibiotic accesses the inner membrane (IM) by including hydrophilic groups in the fatty acid chains18. In addition, Sabnis et al19 demonstrated that modified LPS precursors that would be transported from the IM to the OM are also target of colistin, leading to cell lysis17. Polymyxin E, known as colistin, is a potent clinical antibiotic whose use nearly ceased in the early 1990s due to nephrotoxicity and neurotoxicity. In recent years, it has returned as a last resort antibiotic, due to its effectiveness against multi-drug resistant Gram-negative pathogens17. The veterinary use of colistin allows for the selection of of colistin resistance acquisition in zoonotic bacteria strains, such as non-typhoidal serovars of Salmonella enterica, and this mediates the spread of resistance mechanisms along the food chain20.
PhoP/PhoQ TCS activates the expression of genes that introduce modifications in LPS. This allows bacteria to counteract the bactericidal effect of polymyxins. In the presence of sub-inhibitory concentrations of colistin, the system promotes the expression of pmrD, whose gene product activates the PmrA/PmrB TCS and induces polymyxin resistance genes (ugd, pmrCAB, pgbPE)12.
Lipid A is the LPS target of the PhoP/PhoQ-dependent modifications: (1) introduction of 4-amino-4-deoxy-L-arabinose (L-Ara4N) in the phosphate at position 4, controlled by the pmr, arn or pbg operons12 and (2) introduction of phosphoethanolamine (PEtN) in the position 1-phosphate, controlled by pmrC21,22 Ugd, an UDP-glucose dehydrogenase under PhoP, PmrA and Rcs-dependent regulation, plays a crucial role in L-Ara4N pathway since it converts UDP-glucose to UDP-glucuronic acid, the substrate for the arn pathway23,24.
In this study, we demonstrate how the quinazoline CA439 attenuates the expression of genes that define colistin resistance and thus, it increases colistin efficacy. The quinazoline-mediated enhancement of the polymyxin antibiotic capacity does not only rely on the PhoP/PhoQ-dependent resistance mechanisms inactivation but also on the concomitant alteration of electrochemical properties of the bacterial membrane. The dual treatment attenuates Salmonella virulence in an in vivo model of infection. In sum, our results position the combined colistin-quinazoline use as a promising option to develop a therapeutic strategy to fight against Salmonella infections.
Results
CA439 potentiates the bactericidal effect of colistin
Salmonella typhimurium ATCC 14028 (STM14028) was used as a study model throughout this work. 4-anilinoquinazoline-based compounds down-regulate the activity of the S. typhimurium PhoP/PhoQ system by acting as competitive inhibitors of ATP in the PhoQ autophosphorylation reaction16. We selected CA439 (GI262866A) as representative of these quinazolines (synthesized as previously described16) to evaluate its ability to potentiate colistin activity. All assays were performed in LB, a low Mg2+ medium that ensures the PhoP/PhoQ system with an inducing environmental condition7,8,9,10. CA439 effect was evaluated up to 25 μM, a sub-inhibitory concentration for Salmonella growth capacity that showed a repressive effect over PhoP/PhoQ activity16. The checkerboard assay was employed in which the fractional inhibitory concentration (FIC) was calculated25. The dose-dependent enhancing effect of colistin by CA439 reduced the MIC of colistin from 2.5 μg mL−1 to 0.312 µg mL−1, and resulted in a FIC of 0.125 (Fig. 1a, left). This was corroborated by counting colony-forming units (Fig. 1a, right). None of the CA439-analogues (CA176, CA209, CA454 and CA490, previously synthesized and characterized16) that exerted no repressive effect over PhoP/PhoQ activity showed a colistin-enhancing effect (Fig. 1b), reinforcing that the effect of CA439 selectively targets PhoQ histidine kinase….