Abstract
A growing body of evidence suggests that dysbiosis of the human gut microbiota is associated with neurodegenerative diseases like Alzheimer’s disease (AD) via neuroinflammatory processes across the microbiota-gut-brain axis. The gut microbiota affects brain health through the secretion of toxins and short-chain fatty acids, which modulates gut permeability and numerous immune functions. Observational studies indicate that AD patients have reduced microbiome diversity, which could contribute to the pathogenesis of the disease. Uncovering the genetic basis of microbial abundance and its effect on AD could suggest lifestyle changes that may reduce an individual’s risk for the disease. Using the largest genome-wide association study of gut microbiota genera from the MiBioGen consortium, we used polygenic risk score (PRS) analyses with the “best-fit” model implemented in PRSice-2 and determined the genetic correlation between 119 genera and AD in a discovery sample (ADc12 case/control: 1278/1293). To confirm the results from the discovery sample, we next repeated the PRS analysis in a replication sample (GenADA case/control: 799/778) and then performed a meta-analysis with the PRS results from both samples. Finally, we conducted a linear regression analysis to assess the correlation between the PRSs for the significant genera and the APOE genotypes. In the discovery sample, 20 gut microbiota genera were initially identified as genetically associated with AD case/control status. Of these 20, three genera (Eubacterium fissicatena as a protective factor, Collinsella, and Veillonella as a risk factor) were independently significant in the replication sample. Meta-analysis with discovery and replication samples confirmed that ten genera had a significant correlation with AD, four of which were significantly associated with the APOE rs429358 risk allele in a direction consistent with their protective/risk designation in AD association. Notably, the proinflammatory genus Collinsella, identified as a risk factor for AD, was positively correlated with the APOE rs429358 risk allele in both samples. Overall, the host genetic factors influencing the abundance of ten genera are significantly associated with AD, suggesting that these genera may serve as biomarkers and targets for AD treatment and intervention. Our results highlight that proinflammatory gut microbiota might promote AD development through interaction with APOE. Larger datasets and functional studies are required to understand their causal relationships.
Introduction
Alzheimer’s disease (AD), the most common form of dementia, is a neurodegenerative disorder characterized by a multitude of pathological and clinical hallmarks such as a progressive decline in cognitive function and the buildup of toxic β-amyloid and tau proteins1,2. Due to the growing elderly population worldwide, the number of individuals with dementia is projected to reach 150 million globally by the year 20503. Despite this growing burden on world health, the mechanisms underlying the disease pathology are not fully understood, impeding the development of optimally effective treatments4. Neuroinflammation has emerged as a key feature of AD with mechanistic and treatment implications due to the central role of microglia and inflammation in brain health5,6. There remains an urgent need to understand the genetic risk factors and pathological basis of neuroinflammation in AD so that individuals with a higher risk can be identified for earlier intervention.
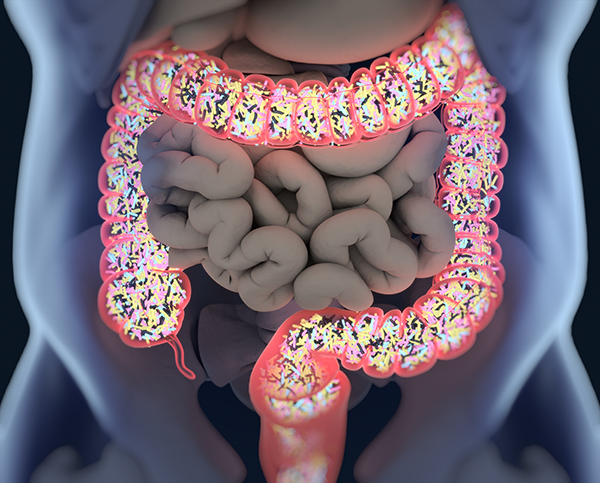
Recently, an association between dysbiosis of the gut microbiome and neuroinflammation has been hypothesized to drive AD. The gut microbiota comprises a complex community of microorganism species that reside in our gastrointestinal ecosystem; alterations in the gut microbiota have been reported to influence not only various gut disorders but also brain disorders such as AD7,8. The human gut microbiota has been suggested to modulate brain function and behavior via the microbiota-gut-brain axis (MGBA), a bidirectional communication system connecting neural, immune, endocrine, and metabolic pathways9. Observational studies across multiple countries show reductions in gut microbiota diversity in AD patients compared to cognitively normal controls10,11,12. Current research indicates that bacteria populating the gut microbiota are capable of releasing lipopolysaccharide (LPS) and amyloids, which may induce microglial activation in the brain and contribute to the production of proinflammatory cytokines associated with the pathogenesis of AD13. The secretion of these biomolecules also harms the integrity of the MGBA and blood–brain barrier (BBB), which worsens with increasing dysbiosis8,14. The composition of the human gut microbiota and risk for AD have been suggested as heritable traits2,15. Apolipoprotein E ε4 (APOE ε4), the most well-established risk gene for AD, has recently been shown to correlate with microbiome composition in humans and mouse models of AD16,17,18. However, few studies have explored the correlation between APOE alleles and microbiome taxa at the human genomic level. In this study, we aim to determine the genetic correlation between the abundance of gut microbial genera and AD diagnosis. We further investigate whether gut microbial genera are correlated with APOE genotyping.
One promising approach to exploring this relationship is the use of polygenic risk score (PRS) analyses. A PRS is an overall estimate of an individual’s genetic liability for a specific trait. The software PRSice-2 is designed to calculate the PRS of an individual by aggregating and quantifying the effect of many single nucleotide polymorphisms (SNPs) in their genome, which are weighted by the effect sizes of each SNP derived from genome-wide association studies (GWASs)19. This approach has previously been used to explore the genetic relationship between gut microbial abundance and complex traits like bone mineral density, rheumatoid arthritis, and depression20,21,22. In the present study, we used this approach to determine the genetic relationship between 119 microbial genera and AD diagnosis. With the largest GWAS of the human gut microbiota23, we first conducted PRS analyses in an AD discovery sample to identify the genera genetically correlated with AD. We then verified our results in a replication sample and meta-analysis with the two samples. The correlation between the top ten significant genera and the APOE genotypes was further analyzed by linear regression analysis.
Materials and methods
Study design overview
The overall design of our study is shown in Fig. 1. Briefly, we used PRSice-219 to calculate PRSs for individuals from our discovery sample. PRSs were calculated based on the summary statistics for 119 microbial genera from the MiBioGen consortium. The significant association between genera and AD diagnosis was determined when the “best-fit” PRS model had a Bonferroni-corrected p < 0.00042 (0.05/119 = 0.00042). We then replicated the results in an independent sample. We conducted logistic regression analyses between the PRSs of associated genera and AD diagnosis to generate relative odds ratios (ORs) for meta-analysis. The multivariate logistic regression model was used to determine whether sex, age, and APOE genotypes affected the correlation between the PRSs of the associated genera and AD diagnosis. Furthermore, we conducted a linear regression analysis to evaluate the genetic association between the PRSs of ten significant genera and the APOE genotypes of individuals in our discovery and replication samples. This study was approved by our institutional review board (IRB) at the University of Nevada Las Vegas (UNLV)….