Abstract
Exposure to environmental pollutants and human microbiome composition are important predisposition factors for tumour development1,2. Similar to drug molecules, pollutants are typically metabolized in the body, which can change their carcinogenic potential and affect tissue distribution through altered toxicokinetics3. Although recent studies demonstrated that human-associated microorganisms can chemically convert a wide range of xenobiotics and influence the profile and tissue exposure of resulting metabolites4,5, the effect of microbial biotransformation on chemical-induced tumour development remains unclear. Here we show that the depletion of the gut microbiota affects the toxicokinetics of nitrosamines, which markedly reduces the development and severity of nitrosamine-induced urinary bladder cancer in mice6,7. We causally linked this carcinogen biotransformation to specific gut bacterial isolates in vitro and in vivo using individualized bacterial culture collections and gnotobiotic mouse models, respectively. We tested gut communities from different human donors to demonstrate that microbial carcinogen metabolism varies between individuals and we showed that this metabolic activity applies to structurally related nitrosamine carcinogens. Altogether, these results indicate that gut microbiota carcinogen metabolism may be a contributing factor for chemical-induced carcinogenesis, which could open avenues to target the microbiome for improved predisposition risk assessment and prevention of cancer.
Main
Increasing evidence suggests that human-associated microorganisms, collectively called the human microbiota, play an important role in cancer development and progression8,9. Although the molecular mechanisms of microbial contributions to cancer development remain largely unknown, translocation of tumour-inducing bacteria from the gut into tissues and microbial production of genotoxins (that is, colibactin) have been demonstrated to induce cancer development10,11. Another important carcinogenic mechanism is the exposure to environmental pollutants, which are often further metabolized after entering the human body3. Contaminant-metabolizing human enzymes, such as cytochrome P450 enzymes, have been well described for their capacity to convert a broad variety of carcinogens, which can lead to their activation or inactivation12. Recent studies have demonstrated that human gut bacteria also have a large potential to metabolize chemically diverse compounds, such as medical drugs, and that the resulting products can get distributed to distal tissues4,5. This led us to investigate whether the gut microbiota could contribute to tumour onset and development through the metabolism of environmental carcinogens.
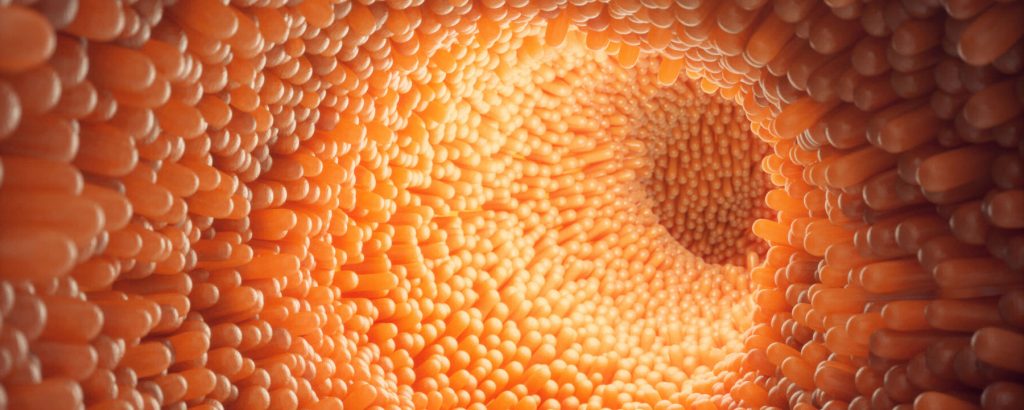
We exemplarily studied bladder cancer, the tenth most common cancer worldwide with high recurrence and progression rates in its invasive form13, whose major risk factors are environmental and occupational exposure to carcinogens14. Nitrosamine compounds, such as N-butyl-N-(4-hydroxybutyl)-nitrosamine (BBN) and related organic contaminants in tobacco smoke, have been well described to induce bladder cancer6. In fact, chronic exposure to BBN is routinely used to induce bladder cancer in rodent models7. Following oral administration, BBN undergoes substantial metabolism through oxidation and glucuronide conjugation. Notably, N-butyl-N-(3-carboxypropyl)-nitrosamine (BCPN), the oxidation product of BBN, induces tumorigenesis through DNA adduct formation in the urothelium6,15. We utilized the BBN-induced bladder cancer mouse model to investigate the contribution of the gut microbiota to chemically induced tumorigenesis as well as its role in toxicokinetics (Fig. 1a).
Antibiotics reduce bladder tumours
To test for possible gut microbiota contributions to BBN-induced bladder cancer development, we compared bladder tumour pathology of antibiotic (ABX)-treated and non-treated C57BL/6 mice with concomitant BBN administration through drinking water (0.05% v/v). We confirmed a reduction of the bacterial load in the gut following ABX treatment through colony-forming unit counting, which was 99.99% lower in treated versus non-treated animals (Extended Data Fig. 1a and Supplementary Table 1). Additionally, 16S rRNA amplicon sequencing demonstrated that ABX treatment, but not BBN administration, significantly reduced gut microbiome α-diversity (measured as observed number of species: Kruskal–Wallis test, P value 0.008134; or as Shannon diversity: Kruskal–Wallis test, P value 4.86 × 10−5), and significantly altered the overall community composition (permutational multivariate analysis of variance test statistic 699.172, P value 0.001, 999 permutations; Extended Data Fig. 1b–d and Supplementary Table 2). After 12 weeks of continuous exposure to BBN in drinking water, BBN was removed for 8 weeks and blinded pathological analysis of urinary bladders was carried out (Fig. 1b and Supplementary Data 1). Notably, most mice with reduced gut bacterial load (ABX–BBN group) were completely free of bladder tumour pathology (81%, n = 26/32), whereas 77% of the control mice without ABX treatment (BBN group) developed neoplastic changes in their bladder tissue (n = 23/30, χ2 test, P value = 1.6 × 10−5; Fig. 1c and Supplementary Table 3). Moreover, invasive tumours, the most aggressive tumour presentation, were found in 53% (n = 16/30, χ2 test, P value = 1.5 × 10−3) of mice in the BBN group, but only in 12% (n = 4/32) of the ABX–BBN group. These results indicated that the gut microbiota may enhance bladder cancer development in BBN-exposed mice.
Next we examined whether contributions of the gut microbiota to bladder cancer development lie in altered urothelial tissue exposure to the administered carcinogen. Using liquid chromatography-coupled mass spectrometry quantification, we found that concentrations of BCPN, but not BBN, in bladder tissue of ABX–BBN-treated mice were significantly lower (P value = 2.31 × 10−3) than in BBN-treated mice during the 12 weeks of BBN exposure (Fig. 1d and Supplementary Table 4). Additionally, we quantified urinary elimination of BBN and BCPN in metabolic cages over 24 h. These measurements demonstrated that urinary BCPN elimination was significantly (P value = 2.33 × 10−3) lower in the ABX–BBN compared to BBN mice, whereas BBN elimination was comparable between the two mouse groups (Fig. 1e and Supplementary Table 5). These results link the observed decrease of tumorigenesis following reduction of the gut bacterial load to decreased urinary BCPN elimination and urothelial BCPN exposure.
BCPN is produced in the intestinal tract
To elucidate possible links between the gut microbiota and BCPN production, we quantified BCPN in nine additional body compartments (plasma, liver, kidney, duodenum, jejunum, ileum, caecum, colon and rectum) of BBN and ABX–BBN-treated animals after 3 and 7 weeks of BBN exposure (Fig. 1a). Whereas we did not detect any difference in BCPN concentrations in plasma, liver and kidney between the two groups of mice (Fig. 2a, Extended Data Fig. 2a and Supplementary Tables 6 and 12), BCPN accumulated in caecum and colon luminal contents of BBN-treated, but not ABX–BBN-treated, animals (Fig. 2b, Extended Data Fig. 2b and Supplementary Tables 7, 9, 13 and 14). We also observed that BCPN levels decrease from caecum to rectum, suggesting BCPN reabsorption from the lower intestine. To control for the effect of ABX on host BBN metabolism, we treated germ-free mice with BBN in drinking water for 10 days with or without ABX treatment and compared BCPN levels in bladder, liver, kidney, plasma and caecum. BCPN levels in all of these tissues were comparable with or without ABX treatment (Extended Data Fig. 2d and Supplementary Table 15) suggesting that BBN metabolism and toxicokinetics is not affected by ABX. To directly test for potential effects of ABX on host BBN metabolism, we measured hepatic BBN to BCPN conversion in HEP-G2 cells, and found it to be unaffected by the addition of ABX (Extended Data Fig. 2e and Supplementary Table 16). These control experiments consolidated our hypothesis that the difference in BCPN levels between the BBN- and ABX–BBN-treated animals is not caused by ABX, but that BCPN is produced in a microbiome-dependent manner in the lower intestine….