Abstract
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the second leading cause of cancer worldwide. Despite approvals of several therapeutics to treat advanced HCC in the past few years, the impact of anti-angiogenic treatment on HCC patient overall survival remains limited. This suggests there may be alternative, perfusion-independent roles of endothelial cells that support tumor progression. Thus, we leveraged a well-defined hydrogel system to establish co-culture models to mimic and characterize the angiocrine crosstalk between HCC and endothelial cells in vitro. Co-cultures of HCC cell lines or patient-derived xenograft organoids with endothelial cells exhibited the upregulation of MCP-1, IL-8 and CXCL16, suggesting that the HCC-endothelial interactions established in our models recapitulate known angiocrine signaling. Additionally, by subjecting co-cultures and mono-cultures to RNA sequencing, transcriptomic analysis revealed an upregulation in the expression of genes associated with tumor necrosis factor (TNF) signaling, such as that of chemokines, suggesting that endothelial cells induce HCC cells to generate an inflammatory microenvironment by recruiting immune cells. Finally, HCC-endothelial angiocrine crosstalk in the co-culture models polarized macrophages towards a pro-inflammatory and pro-angiogenic phenotype, paralleling a tumor-associated macrophage subset previously reported in HCC. Together, these findings suggest that these HCC-endothelial co-culture models may serve as important models to understand and target the interplay between angiogenesis and the immune milieu.
Introduction
The process of angiogenesis enables tumor expansion through blood vessels, which serve as physical conduits to meet metabolic demands of the growing tumor [1]. However, angiogenesis inhibitors typically only confer a transient period of clinical benefit, following which the tumor resumes growth [2]. This suggests there may be alternative, perfusion-independent roles of endothelial cells that support tumor progression [3]. Indeed, it is now increasingly recognized that endothelial cells confer many growth advantages to cancer cells through the production of growth factors and trophogens, commonly referred to as angiocrine factors [3], which can influence cancer proliferation, stemness, epithelial-to-mesenchymal transition, invasiveness and immunosuppression [4]. Understanding the angiocrine function of endothelial cells may generate new therapeutic targets to control tumor development.
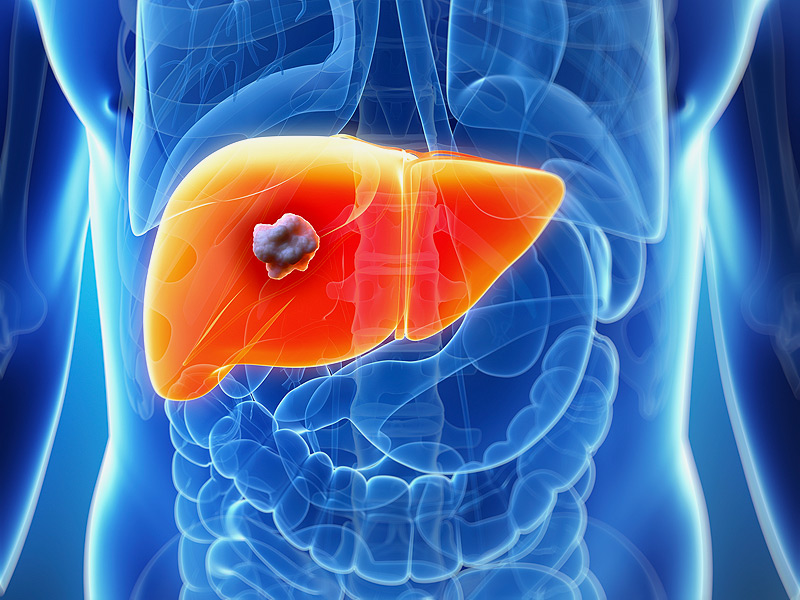
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the second leading cause of cancer worldwide [5]. Despite advances in the diagnosis and treatment of the disease, prognosis of HCC patients remains dismal, with a 5-year overall survival rate of less than 20% [6]. Given that HCC tumors are generally highly vascularized and many pro-angiogenic growth factors are over-expressed, therapeutic options are based on the inhibition of angiogenesis, such as the use of small molecule kinase inhibitors that target various tyrosine kinases associated with neo-vascularization [[7], [8], [9]]. Although several therapeutics have been approved in the past few years to treat advanced HCC, the impact of anti-angiogenic treatment on HCC patient overall survival remains limited. A recent clinical trial in patients with unresectable HCC demonstrated that the combination of immunotherapy with anti-angiogenic treatment was more effective than standard-of-care treatment with the tyrosine kinase inhibitor Sorafenib in prolonging overall survival at 12 months and progression-free survival outcomes [10]. In addition, we have previously shown that there is re-emergence of fetal-associated PLVAP+/VEGFR2+ endothelial cells and embryonic-like FOLR2+/CD163+ tumor-associated macrophages (TAMs) in HCC and this immunosuppressive environment was found to be maintained by VEGF/NOTCH signaling [11]. These findings suggest that there may be critical functions of endothelial cells beyond their known structural role in forming blood vessels. They may serve as a source of angiocrine factors that act on cancer and other stromal cells in the tumor microenvironment [4]. However, the role of angiocrine factors in modulating HCC progression remains unclear.
In this study, to mimic the angiocrine crosstalk in HCC, we developed and carefully characterized HCC-endothelial co-culture models, comprising HCC cell line-derived spheroids or HCC patient-derived xenograft (PDX)-derived organoids grown with endothelial cells. While other studies have previously reported the development of HCC-endothelial co-culture models [[12], [13], [14]], these models typically only focused on model development using immortalized HCC cell lines (not patient-derived organoids), characterized endothelial network formation and used these models for drug screening. To address the need for HCC-endothelial co-culture models to elucidate the effect of angiocrine signaling on the HCC transcriptome, we leveraged our previous experience in culturing HCC PDX-derived organoids in vitro using macroporous hydrogels [15] to enable the co-culture of endothelial cells with HCC PDX-derived organoids. We hypothesized that hydrogels incorporating integrin-binding sites and matrix metalloproteinase (MMP)-sensitive domains would be suitable matrices, given that similar hydrogel systems were previously shown to be conducive for the culture of cancer organoids [16,17] and endothelial cells [18,19]. We report that in the absence of exogeneous angiogenic factors typically added to endothelial cell cultures in hydrogels, hyaluronan (HA)-based hydrogels that permit integrin-mediated adhesion and MMP-mediated matrix degradation support the co-culture of several HCC PDX-derived organoids with endothelial cells. Using these co-culture models, not only were certain angiocrine factors which have known roles in recruiting myeloid cells upregulated [4], we also found that endothelial cells induced an inflammatory phenotype in HCC cells involving the tumor necrosis factor (TNF) signaling pathway. Importantly, the interaction between HCC and endothelial cells promoted the generation of pro-angiogenic and inflammatory macrophages in tri-culture, mimicking the HCC tumor milieu [20].