Highlights
- •iPSC-derived hypoimmunogenic CTLs exhibit robust cytotoxicity against cervical cancer
- •These rejuvenated CTLs are highly enriched with tissue resident memory T cells
- •It would provide a promising approach to “off-the-shelf” T cell therapy
Summary
Functionally rejuvenated human papilloma virus-specific cytotoxic T lymphocytes (HPV-rejTs) generated from induced pluripotent stem cells robustly suppress cervical cancer. However, autologous rejT generation is time consuming, leading to difficulty in treating patients with advanced cancer. Although use of allogeneic HPV-rejTs can obviate this, the major obstacle is rejection by the patient immune system. To overcome this, we develop HLA-A24&-E dual integrated HPV-rejTs after erasing HLA class I antigens. These rejTs effectively suppress recipient immune rejection while maintaining more robust cytotoxicity than original cytotoxic T lymphocytes. Single-cell RNA sequencing performed to gain deeper insights reveal that HPV-rejTs are highly enriched with tissue resident memory T cells, which enhance cytotoxicity against cervical cancer through TGFβR signaling, with increased CD103 expression. Genes associated with the immunological synapse also are upregulated, suggesting that these features promote stronger activation of T cell receptor (TCR) and increased TCR-mediated target cell death. We believe that our work will contribute to feasible “off-the-shelf” T cell therapy with robust anti-cervical cancer effects.
Introduction
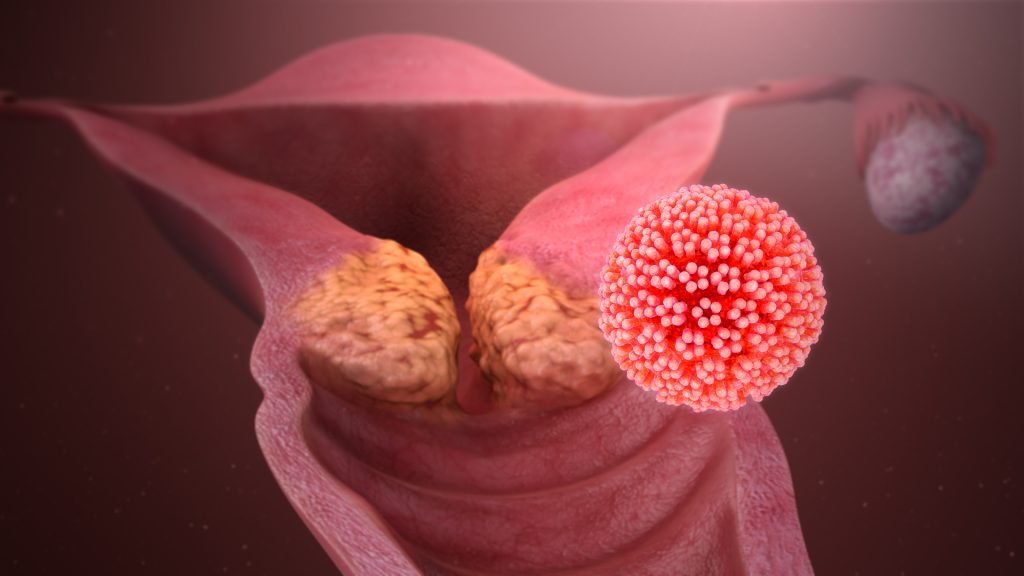
Cervical cancer is one of the most common malignancies in women worldwide. In 2020, ∼604,000 women were diagnosed with cervical cancer globally; more than 341,000 died from cervical cancer.1 Cervical cancer harbors high-risk human papilloma virus (HPV) in 99% of cases, with HPV16 accounting for 50%–60% and HPV18 accounting for ∼20%.
Although prophylactic HPV vaccines can prevent initial infection by high-risk HPV types, these vaccines are not effective against established cancers.2,8,9 In early-stage disease, total hysterectomy is indicated, which abolishes fertility and increases long-term risks for cardiovascular disease even with ovarian conservation.10 Metastatic and relapsed cervical cancer is generally incurable. It also is highly refractory to chemotherapy, especially in young women.11,12,13,14 Development of effective cervical cancer treatment thus remains urgent. As cervical cancer cells constitutively express E6 and E7 oncoproteins (contributors to tumorigenesis and cancer cell survival), E6 and E7 are attractive treatment targets.2,3,4,5,6,7,8,9,11,12,13,14
We demonstrated that induced pluripotent stem cell (iPSC)-derived HPV16 E6-specific cytotoxic T lymphocytes (CTLs) robustly suppress cervical cancer.15 Although antigen-specific CTL therapy can induce durable remission in selected tumors such as melanoma,16 CTLs are chronically exposed to tumor antigens, resulting in exhaustion.17,18 Functionally rejuvenated CTLs generated from iPSCs (rejuvenated CTLs [rejTs]) include stem cell memory and central memory phenotypes and persist long term in vivo, resulting in continuous tumor elimination by an invigorated immune system.15,19,20,21 The greatest advantage of rejT therapy is that once iPSCs are established from an antigen-specific CTL clone, unlimited numbers of therapeutic T cells can be generated.
However, generating rejTs from individual patients is time consuming and unrealistically expensive. Allogeneic T cell therapy banks can solve both those problems but do not overcome the two major obstacles to allogeneic T cell therapy: graft-versus-host disease and host-versus-graft disease. In immunocompetent cervical cancer patients, the dominant problem is rejection of foreign T cells by alloreactive recipient CD8+ T cells (host-versus-graft disease). Although β2-microglobulin (B2M) disruption can erase human leukocyte antigen (HLA) class I expression to evade immunorejection by CD8+ T cells,22 recipient natural killer (NK) cells attack the HLA class I-negative cells. CRISPR-Cas9 gene-editing approaches to reduce NK cell attack include overexpression of HLA-E, which binds to NKG2A23; expression of CD47, a “don’t eat-me” signal24; expression of HLA-G, an NK cell inhibitory ligand25; and HLA-C retention for binding to the inhibitory receptor killer cell immunoglobulin-like receptor.26 However, since work using these methods has not demonstrated evasion of recipient immune reaction against iPSC-derived T cells, whether they apply in allogeneic T cell therapy is uncertain. Use of iPSC-derived chimeric antigen receptor T cells (CARTs) with forced expression of HLA-E after triple knockout (HLA class I, class II, PVR) yielded alloimmune suppression. Unfortunately, T cell function and killing function of gene-edited CARTs were not thoroughly evaluated.27 Our study addressed these issues by using iPSC-derived HPV16 E6-specific CTLs targeting cervical cancer.
While CTLs, unlike CARTs, can recognize intracellular antigens, major histocompatibility complex (MHC) restriction on the T cell receptor (TCR) limits CTL deployment: it precludes generation of universal CTLs that could be used for all patients. However, gene editing to suppress recipient allogeneic immune reaction will permit treatment of many patients with CTLs generated from a single iPSC line. For example, if MHC binding of rejTs is mediated by HLA-A24, then only patients expressing HLA-A24 are eligible for treatment using rejTs that express HLA-A24 and thereby will be protected from attack by host T cells or NK cells. HLA-A24 is present in ∼60% of South American and Eastern Asian populations and in ∼30% of North American and European populations. With rejTs restricted by HLA-A24 and HLA-A02, achieved coverage in South America and Eastern Asia should be ∼80% and in North America and Europe ∼70%. This report thus aims to establish a proof of concept for “off-the-shelf” T cell therapy limited to specific HLA types, i.e., “limited off-the-shelf” T cell therapy.
We prioritized expressing HLA-A24 on HPV-rejTs both because we hoped to suppress NK cells via binding of the Bw4 ligand to KIR3DL1 and because HLA-A24 restriction already exists on HPV-rejTs. We also integrated a B2M-HLA-E fusion construct, expecting to inhibit NKG2A+ NK cells by HLA-E/NKG2A binding. Using CRISPR-Cas9 technology, we successfully generated HLA class I-edited HPV-rejTs with dual integration of HLA-A24 and HLA-E and lacking expression of other class I molecules. These were not rejected by recipient CD8+ T cells and could evade NK cell attack. Furthermore, these rejTs, which were enriched with tissue resident memory T cells (TRM), could maintain robust suppression of cervical cancer even without peptide-pulse treatment; those of the original CTL clone could not. We accordingly propose that HLA-engineered HPV-rejTs using this method provide a sustainable and promising approach to successful “off-the-shelf” T cell therapy in overcoming cervical cancer.
Results
CRISPR-Cas9 “scarless” technology successfully edited HLA class I antigen expression by iPSCs
To edit HLA class I antigens efficiently and safely, we used CRISPR-Cas9 two-step “scarless” gene editing, a combination of two-step homologous recombination and positive-negative selection with magnetic beads.28 As this technique does not leave selection markers, alleles can be edited without creating INDELs.28
Our goals were erasure of HLA class I antigens in iPSCs established from an HLA-A2402-restricted HPV16 E6-CTL clone15 and limited expression of HLA class I molecules, thereby evading recipient NK cell attack.
The donor plasmid used in the initial editing (“first edit”) contains a bicistronic cassette that expresses enhanced green fluorescent protein (EGFP) and truncated CD8. EGFP expression permits distinction between left and right homology arms under control of the promoter of UBC, encoding ubiquitin C (Figure 1A). A short hairpin RNA (shRNA) was also introduced to permit negative selection for random integration on the first edit: Expression of shRNA (episomal or randomly integrated) marks cells as negative.28 Table S1 lists primers used for genotyping PCR. They are designed exterior to the left (5′) and right (3′) of each homology arm. Using electroporation we also transfected iPSCs with both the Cas9/guide RNA (gRNA) plasmid and the first-edit donor plasmid. After magnetic-bead selection for CD8 expression, EGFP-expressing cells were identified among the biallelic clones via fluorescent imaging on day 10 (Figure 1B). Biallelic iPSC clones with bright EGFP expression were selected, with integration confirmed using PCR (Figure 1C). For the second edit, a different (“second-edit”) donor plasmid and Cas9/gRNA plasmid were similarly transfected into biallelic iPSCs (Figure 1A). Since the HPV16 E6-rejTs used were HLA-A2402 restricted, we first generated HLA-A2402 single integrated iPSCs (KI-A24-iPSCs). The second-edit donor plasmid was designed to integrate HLA-A2402 cDNA with linker (GGGS×4) on the 5′ side of the B2M stop codon, thereby creating a biallelically integrated B2M-HLA-A24 fusion protein (Figure S1A). After magnetic-bead selection for cells that did not express CD8 and cloning, genotyping confirmed intact integration of HLA-A2402. The non-edited wild-type (WT) PCR product was 7.7 kb long, the first-edit PCR product (biallelic clone) was 10.6 kb long, and the HLA-A2402 integrated PCR product was 8.8 kb long (Figure S1A). To generate HLA-E0103 single integrated iPSCs (KI-E-iPSCs), we used another donor plasmid designed to replace the endogenous B2M locus with an exogenous B2M-HLA-E fusion construct, thereby creating a biallelically integrated B2M-HLA-E trimer fusion protein (Figure S1B). For the second edit, a different (“second-edit”) donor plasmid (for HLA-E integration) and the Cas9/gRNA plasmid were similarly transfected into biallelic iPSCs. After magnetic-bead selection for cells that did not express CD8-negative selection and cloning, PCR genotyping showed that the WT PCR product was 7.7 kb long, while the HLA-E0103 integrated PCR product was 4.4 kb long (Figure S1B). Finally, to yield a dual integrated HLA-A24 and B2M-HLA-E fusion construct in each allele, we transfected these two donor plasmids (for HLA-A2402 and HLA-E0103 integration) simultaneously, thereby generating HLA-A2402 and HLA-E0103 dual integrated iPSCs (KI-A24&E-iPSCs) in each allele (Figure S1C). After magnetic-bead selection for cells that did not express CD8 and cloning, PCR genotyping yielded two PCR products, one for HLA-E0103 (4.4 kb long) and one for HLA-A2402 (8.8 kb long). We selected clone #1, in which on gel electrophoresis the presence of both was confirmed (Figure 1D). Sanger sequencing detected no INDELs between homology arms and the integrated sequence in HLA class I-edited iPSCs (Figure S1D)…..