Tumors can be divided into ‘hot’ (T cell inflamed) or ‘cold’ (T cell noninflamed) according to the presence of immune cells. In this review, we discuss variables that influence T cell migration into the tumor microenvironment. Chemokines can attract T cells to the tumor site and tumor intrinsic pathways can influence the composition of local chemokines. Tumor-induced vasculature can hamper T cell migration. Other immune cells and tumor-derived molecules can block T cell proliferation and survival. It is important to better understand these mechanisms in order to target them therapeutically. Enhancing T cell infiltration may increase response rates to immunotherapy and increase survival.
Trends
Cancer immunotherapy is a rapidly evolving field. Despite promising results, long-lasting response rates remain around 20–40%.
The immune cell landscape in tumors is heterogeneous across patients and can influence prognosis and outcome of immunotherapy.
It is important to investigate mechanisms that underlie migration of immune cells into the TME.
Drugs are being tested in preclinical models and clinical trials that can manipulate the immune cell landscape within the TME. These can be used as monotherapy, but more likely in combination with other therapies.
Tumor Microenvironment: ‘Hot’ versus ‘Cold’ Tumors
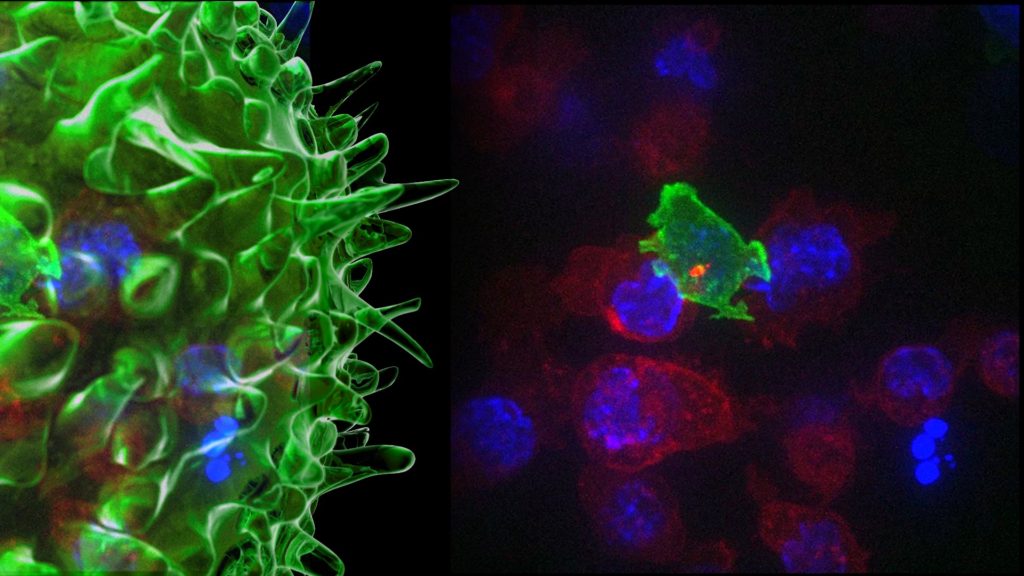
Tumors develop under constant vigilance of the immune system and are able to thrive by evading the antitumor immune response. Research has therefore shifted towards a better understanding of the immune cell landscape of the tumor microenvironment (TME, see Glossary) that shapes this immune response (Box 1) [1]. Main immune cell players within the TME are T-helper cells, cytotoxic T cells (CTLs), T-regulatory cells (Tregs), natural killer (NK) cells, macrophages, dendritic cells (DCs), granulocytes, B cells, and myeloid-derived suppressor cells (MDSCs). However, heterogeneity regarding immune cell infiltrates in tumors is observed between patients.
Tumors can be roughly divided in so-called hot (T cell inflamed) and cold (T cell noninflamed) tumors [2, 3, 4]. Hot tumors have an abundance of tumor-infiltrating lymphocytes (TILs), and exhibit an initial immune response that is dampened by upregulation of immune checkpoints or increased numbers of suppressive immune cells. By contrast, cold tumors are defined by the absence of a sufficient population of pre-existing TILs. Cold tumors can be further subdivided into the immune-excluded phenotype and the immunologically ignorant phenotype (Figure 1) [5]. This illustrates that there are multiple causes for a tumor to be cold. In the immunologically ignorant phenotype there seems to be no activation and recruitment of T cells at all, whereas in the immune-excluded phenotype T cells are attracted to the periphery of the tumor but fail to penetrate.
The pre-existing immune landscape within the TME seems to be of prognostic value in multiple malignancies [6], and may serve as a predictive biomarker of response to different types of immunotherapy, such as immune checkpoint inhibition [7, 8] and DC vaccination [9]. Even adoptive T cell therapy, which relies on harvesting tumor-specific T cells to reinfuse them after activation and expansion, has partial response rates due to the inability of T cells to infiltrate the tumor [10]. Since current immunotherapies are aimed at enhancing and supporting the body’s own antitumor immune response, offering immunotherapy to patients without pre-existing TILs appears to be ineffective.
The heterogeneity of immune cells infiltrating the TME that is observed among patients warrants the study of the underlying mechanisms that determine whether a tumor is hot or cold; especially considering the prognostic and predictive significance. In this review we discuss different factors that affect immune cell migration into the TME, with a focus on T cells, and that may constitute targets for therapies designed to enhance T cell infiltration and effective tumor responses. We discuss the role of chemokines, endothelium, local granulocytes, and other factors influencing T cell survival, and propose an integrative approach to simultaneously asses all these contributing factors of T cell migration in cancer patients (Figure 2, Key Figure).
Chemokines: Providing a ‘ZIP Code’ for T Cells
Cells migrate in response to various environmental cues. Chemokines can act as a ‘ZIP code’ for T cells and other immune cells. Immune cells express a variety of chemokine receptors for chemotaxis and selectin ligands to bind to blood vessels and migrate into surrounding tissues. Naïve T cells express a set of homing receptors that is different from those of effector or memory T cells. Through the expression of L-selectin and chemokine CC receptor (CCR)7, naïve T cells home to lymphoid tissues and are exposed to their cognate ligand. After stimulation and differentiation in the lymphoid tissue, this homing receptor profile of T cells is altered, and this enables mature T cells to find their specific targets. The loss of CCR7 allows effector T cells to migrate to nonlymphoid tissues. Each target tissue has a specific set of ligands that interact with corresponding receptors on T cell subsets, of which homing to skin and gut have been extensively investigated [11].
The TME also produces a specific offset of cytokines and chemokines for homing T cells. Gene expression profiles of chemokines and immune cell infiltration have been investigated in different tumor types. Consistently, expression of chemokine CXC ligand (CXCL)9 and CXCL10 is correlated with immune cell infiltration [12, 13, 14, 15, 16, 17]. Chemokine CC ligand (CCL)2 and CCL5 are also positively associated with infiltration [17, 18], although a negative influence of these chemokines on migration of T cells to the TME has also been found [14]. CD8+ effector cells upregulate cognate chemokine receptors, but only chemokine CXC receptor (CXCR)3-mediated signaling (the key receptor for CXCL9 and CXCL10) is nonredundant for the extravasation of adoptively transferred CD8+ T cells across tumor vasculature [19]. Upregulation of CXCL9 seems to have a favorable effect on T cell tumor infiltrates in preclinical models. However, there are concerns regarding a possible dual effect of the CXCL9–CXCR3 axis in facilitating T cell migration and metastasis of tumor cells [20]. High expression of CCL2, CCL22, and CXCL12 attract immunosuppressive Tregs and MDSCs [13]. CCL2 blockade reduces immunosuppression and augments cancer immunotherapy in mouse models of non-small cell lung cancer (NSCLC) [21]. Ex vivo treatment of prostate cancer explants with poly-I:C, interferon-alpha (IFNα) and celecoxib (PAC) is able to induce expression of CXCL9, CXCL10, and CCL5, resulting in T cell infiltration in a preclinical model for prostate cancer [13]. This might be an interesting candidate for combination therapy, as cold tumors can be reshaped into hot tumors, and become more susceptible to current immunotherapies. Other chemokines that previously have been associated with T cell infiltration are CX3CL1, CCL3, CCL4, CCL11, and CXCL11 [14, 17].
Besides chemotaxis, tumor-derived chemokines may misdirect activated T cells to stromal cells surrounding the tumor. For example, production of CXCL12 by the stromal cells that surround pancreatic tumors attracts effector T cells to these cells, preventing them from entering the tumor core. Targeting CXCL12 in combination with an antibody blocking programmed death-ligand 1 (PD-L1) showed promising results in mouse models of pancreatic cancer [22]. The majority of chemokine profiles described above are inducible by IFNγ, which is one of the key molecules secreted by effector T cells. Therefore, the presence of activated T cells may induce the recruitment of more effector T cells through a positive feedback loop [23]. In clinical studies of metastatic melanoma, the combination of a peptide-based vaccine with an intralesional injection of IFNγ induced secretion of CXCL10, CXCL11, and CCL5. Consequently, the systemic presence of effector T cells increased, but it did not increase the number of effector T cells within the TME. This might be due to a conflicting effect of secondary immune regulation through induction of IFNγ, leading to upregulation of PD-L1 and indoleamine-2,3-dioxygenase (IDO), which can negatively influence the migration and survival of T cells in the TME [24, 25].
To evade T cell infiltration, tumors can modify their chemokine expression profile in different ways. CCL2 for example, can be nitrosylated by reactive nitrogen species, reducing its chemo-attractive effects on effector T cells, but not on MDSCs [26]. Also other mechanisms can be modified, such as up- or downregulation of signaling pathways and epigenetic remodeling (Box 2). Exploiting the potential of effector T cell-recruiting chemokines is an interesting area of research, however, major hurdles such as toxicity and targeting have yet to be resolved.
Vessels: Roads to the Tumor Microenvironment
The vasculature is pivotal in the trafficking of immune cells to target tissues. Below, we discuss how tumor-induced angiogenesis influences T cell migration and ways to target this process.
Endothelial cells express vascular ligands corresponding to the tissue in which they reside. Tumors influence the type and amount of expressed ligands on tumor endothelium [27]. Under the influence of vascular endothelial growth factor (VEGF) and fibroblast growth factor, adhesion molecules like E-selectin, intercellular adhesion molecule (ICAM)-1/2, vascular cell adhesion molecule (VCAM)-1, and CD34 are downregulated on endothelial cells [28]. This process is called endothelial cell anergy, and results in the inability of T cells to adhere to the tumor vasculature, which prevents them from reaching the tumor. A specialized form of blood vessels called high endothelial venules (HEV) can also be induced by tumors. HEV are associated with tertiary lymphoid structures (TLS) and seem to have a positive influence on T cell migration (Box 3).
Another mechanism by which tumor endothelial cells can inhibit T cell migration is through the establishment of a tumor endothelial death barrier by upregulation of Fas ligand (FasL). This is associated with a decrease of effector T cells and a relative increase in Tregs (which express a higher amount of antiapoptotic genes) within the TME [29]. Preclinical models of ovarian, colon, and renal cancer have revealed that tumor cell-derived VEGF-A, prostaglandin E2, and interleukin (IL)-10 induce the expression of FasL on tumor endothelial cells, which selectively kills effector T cells. Inhibition of VEGF and prostaglandin E2 resulted in downregulation of FasL and CD8+ T cell influx [29].
Under the influence of high levels of tumor-induced VEGF, aberrant leaky vessels are formed. Antiangiogenic therapy was first developed under the assumption that it would block the formation of tumor-induced vessels, thereby starving the tumor of nutrients and depleting it of oxygen. However, a paradoxal effect occurred; the therapy contributed to a tumor-promoting hypoxic microenvironment and decreased T cell infiltration [30]. Lower doses of anti-VEGF may instead induce normalization of vessels, decreasing tumor-promoting hypoxia and increasing accessibility for immune cells and other therapeutic agents to reach the TME [30].
One study showed that low doses of DC101, an anti-VEGF receptor 2 antibody, could normalize tumor vessels, improve overall perfusion, increase T cell infiltration, and decrease tumor hypoxia [31]. Targeting VEGF might therefore be a strategy applied in combination with immunotherapy. In fact, clinical trials are showing promising results. A phase I trial combining the immune checkpoint inhibitor ipilimumab (anti-CTLA4) with the anti-VEGF antibody bevacizumab in patients with metastatic melanoma is well tolerated and results in a median overall survival of 25.1 months compared to 11.2 months in a phase III trial of ipilimumab plus dacarbazine [32, 33]. Tissue samples pre- and post-treatment showed post-treatment morphological changes in tumor endothelium, with higher expression of E-selectin, indicating a higher accessibility to T cells [32]. Further investigation showed that this combination treatment resulted in an increase in adhesion molecules ICAM-1 and VCAM-1, and CXCL10, which increased CD8+ T cell infiltration [34]. Phase I trials exploring various combinations of immune checkpoint inhibitors combined with antiangiogenic agents have also been initiated in patients with different types of cancer. The first clinical results are promising [35] and more are expected in the coming years [36]. Some of the main obstacles are finding the optimal dose and route of administration to obtain a synergistic combination of therapeutic agents. Mathematical tumor models to predict optimal drug regimens may be of value [37].
Granulocytes: Controlling T Cell Traffic
The TME is often associated with immune suppressive cells that negatively affect T cell migration, activation, or proliferation. These cells include macrophages, immature DCs, MDSCs, and Tregs, which are discussed below. However, there are also immune cells that positively affect T cell migration. The role of granulocytes has long been overlooked in tumor immunity, but these cells are also able to influence T cell migration. In these cases the tumor seems to act as a permanent site of inflammation where granulocytes (neutrophils, eosinophils, and basophils) can cause a chronic inflammatory response. This contributes to immune evasion by inhibiting T cell proliferation and attraction of Tregs, and it contributes to tumor growth, remodeling, and paving the way for metastasis. As is widely accepted for macrophages, a similar distinction of type 1 (antitumor) and type 2 (protumor) tumor-associated neutrophils (TANs) has been proposed [38]. However, this distinction is not clear cut and timing seems to be crucial. In the early development of NSCLC, for example, a subset of TANs has been identified that can acquire antigen-presenting cell (APC)-like qualities that stimulate effector T cells to infiltrate the tumor. In later stages of tumor progression however, these cells lose their APC-like properties and revert to an immunosuppressive phenotype [39, 40].
Tumor eosinophilia is associated with a good prognosis for various cancers, but poor clinical outcome was also reported in a few studies [41]. Little is known about the precise nature in which eosinophils influence the tumor–host interaction, but recently it has become clear that they can affect T cell migration. A murine model of melanoma was used to show the different mechanisms by which eosinophils contribute to an antitumor immune response [42]. When Tregs were decreased, an increase in eosinophils was observed, which in turn led to an eosinophil-dependent induction of effector T cell migration into the tumor. This process was mediated by the expression of CCL5, CXCL9, and CXCL10. Eosinophils were also shown to contribute to vascular normalization. Furthermore, the cotransfer of eosinophils and CD8+ T cells skewed tumor-associated macrophages (TAMs) to a type-1-like phenotype, contributing further to an effective antitumor immune response.
Basophilia has been associated with T-helper-2-like responses, and now a similar antitumor role for basophils has been discovered within the TME [43]. When Tregs were completely depleted, intratumoral basophils drastically increased, which in turn enhanced infiltration of CD8+ T cells via the production of CCL3 and CCL4.
Overall, the heterogeneity, plasticity, and multiple roles of granulocytes make them both a challenging but also a promising target for immunotherapy.
Final Destination: Tumor Microenvironment
When studying different mechanisms by which T cells migrate to the TME, it is also important to note that cells must be able to survive and proliferate within the TME to maintain adequate numbers for antitumor immune responses. There are a multitude of mechanisms by which the TME creates a hostile environment for immune cells that leads to T cell exhaustion. The best-known mechanism is through the expression of programmed cell death protein 1 (PD-1) on T cells and PD-L1 on tumor cells. Unlike the name implies, PD-1 does not induce cell death directly, but rather reduces activation, proliferation, and survival factors of T cells [44]. There are some studies observing correlations between PD-L1 expression and a reduced number of TILs [45, 46], however, other studies report no such correlations and different combinations of PD-L1 positivity with or without TILs are prevalent [47, 48]. T cells secreting IFNγ can also induce PD-L1 expression on tumor cells [48], but also IDO expression and attraction of Tregs [49]. Immunotherapy targeting PD-1/PD-L1 reactivates the pre-existing T cell infiltrate within the TME [50]. Blocking the PD-1/PD-L1 pathway might also improve infiltration of T cells into the TME [51, 52]. Expression of PD-L1 on tumors has been associated with good clinical response to PD-1/PD-L1-based immunotherapy in some cancers [53].
Many human cancers can express IDO, which is associated with advanced disease [54]. IDO expression causes immunosuppression through depletion of tryptophan and production of kynurenine [55], which can induce T cell apoptosis. IDO activity also leads to the formation of Tregs and attraction of MDSCs [56]. Many clinical trials are underway using IDO inhibitors in a wide range of cancer types, however, monotherapy might not be sufficient [57]. Strategies using IDO inhibitors combined with immune checkpoint blockade improves effects of monotherapy [58, 59] and are currently tested in clinical trials.
Transforming growth receptor beta (TGF-β) is expressed in a wide variety of cancers by tumor cells, stromal fibroblasts, macrophages, DCs, and immature myeloid cells [60]. TGF-β is mainly associated with inhibition of cell proliferation and can directly inhibit T cell proliferation and activation, while promoting survival of Tregs [60]. Tumor cells themselves often acquire resistance to the antiproliferative effect through mutations or by decreasing the expression of TGF-β receptors [61]. Immunomodulation by TGF-β also results in differentiation of suppressive immune cell phenotypes such as MDSCs, immature and regulatory DCs, which in turn lead to the induction of Tregs [62]. TGF-β expression has also been correlated with a higher infiltration of macrophages into the TME through the induction of chemokines [62].
Attracted MDSCs and macrophages in the TME can produce arginase-1 and inducible nitric oxide synthase 2, which both use l-arginine as a substrate. This causes depletion of L-arginine in the TME and the production of reactive nitrogen species that hamper T cell proliferation and functioning [63]. L-arginine is important for T cell metabolism, and its depletion results in decreased expression of the CD3ζ chain of the T cell receptor, cell cycle arrest and decreased metabolic fitness [63, 64]. In murine breast cancer models, oral administration of l-arginine resulted in reduced tumor growth and increased survival, mediated by increased CD4+ and CD8+ T cells [65]. Furthermore, MDSCs can directly induce T cell apoptosis by the production of galectin 9 that binds T cell immunoglobulin domain and mucin-domain containing-3 (TIM3); a checkpoint molecule that is expressed by exhausted effector T cells [66].
Hypoxia is another feature of the TME that is correlated to poor patient outcome and contributes to decreased effector T cell proliferation and survival [67, 68]. As tumors grow in size, hypoxic microenvironments are formed, which attract MDSCs and TAMs. Tumor cells can secrete high levels of CCL28 under hypoxic conditions; a chemokine that can recruit Tregs to the TME [69]. Tregs can survive in hypoxic conditions and as a response, upregulate CD37 and CD39, which convert ADP and ATP into adenosine. Meanwhile, hypoxia downregulates the reuptake of adenosine, resulting in high levels of extracellular adenosine. Subsequently, adenosine inhibits T cell proliferation and expansion, and secretion of effector cytokines by binding to adenosine A2A receptors on T cells [70]. Furthermore, Tregs can express high levels of the IL-2 receptor, the lymphocyte growth factor. Competition for IL-2 by Tregs can therefore contribute to decreased clonal expansion. However, therapeutic targeting of IL-2 is difficult due to short half-life and systemic toxicity due to cytokine storms [71].
Concluding Remarks
We have discussed the major molecular pathways that can affect T cell migration by tumors and different components of their microenvironment. We have described how T cell migration is influenced by chemokines, tumor-induced vasculature, the presence of suppressive immune cells, including granulocytes, and how T cells can survive in a mainly hostile TME. It is important to note that there are other known and unknown factors influencing T cell migration, such as other lymphocyte subsets (e.g., NK cells and NK-T cells), the microbiome, and previous exposure of the immune system to some viruses.
To enhance efficacy of immunotherapy, it seems to be beneficial to include patients with pre-existing T cell-inflamed tumors. There is a need to find targets for combination therapy, in order to offer the same opportunities to patients with T cell noninflamed tumors (see Outstanding Questions). It is likely that across different types of tumors and even across individuals, different mechanisms may contribute to hampered or enhanced T cell infiltration. Therefore, it is important to investigate whether one specific, or a combination of mechanisms is mostly involved in individual tumors. A multifaceted approach has been proposed in an attempt to find new biomarkers to predict the outcome or choice of immunotherapy, in which mapping of the TME is crucial [2, 72, 73]. To resolve this issue, multiple techniques can be used, which are able to map the TME and the immune cell landscape [74] (Box 4).
We hypothesize that multiplex immunohistochemistry (IHC) can be used to create a so-called immune evasion map (Figure 2) to identify all ongoing mechanisms in a specific tumor, which can then be used as a rational for personalized combination therapies. In patients with hot tumors it might be sufficient to reactivate the pre-existing immune cell infiltrate by combinatorial blocking of checkpoints and inhibiting immunosuppressive molecules. In patients with cold tumors, it will be necessary to first redirect effector T cells towards the tumor by, for example, induction or blocking of some chemoattractants, depletion of suppressive immune cell subsets, or vessel normalization. Recent clinical trials utilizing oncolytic viruses converted cold tumors into hot that were characterized by increased T cell infiltration [75, 76] and by using bispecific antibodies targeting T cells and tumor antigens [77].
Only when the roadmap is complete, traffic jams and obstacles towards the tumor can be solved and T cells can reach the site of the tumor for demolition.
Acknowledgments
The authors would like to thank Felix Fenneman for his illustrations and Kalijn Bol and Jorieke Weiden for critically reading this manuscript. I.J.M.d.V received Vici-918.14.655 from the Netherlands organization for scientific research (NWO). C.G.F. received the NWO Spinoza award, ERC Advanced grant PATHFINDER ( 269019 ) and Dutch Cancer Society KWO award KUN2009-4402. We apologize to all the authors whose work we were unable to cite due to reference limits.