Researchers at the Ludwig-Maximilians-University, the German Center for Neurodegenerative Diseases (DZNE), and the Institute for Stroke and Dementia Research (ISD) in Munich, Germany, have identified a brain inflammation marker in patients at early asymptomatic stages of Alzheimer’s disease. This secreted marker molecule, which can be measured from cerebrospinal fluid taps, may provide clinicians with a rapidly detectable biomarker for the transition from preclinical Alzheimer’s disease to cognitive impairment and progression to full dementia. Such is the conclusion of a multi-center study on a large group of human patients, published online in EMBO Molecular Medicine.
Alzheimer’s disease, an increasing problem in today’s aging populations, is characterized by amyloid peptide plaques and tau protein aggregates in nerve cells. Understanding its molecular causes and risk factors has been challenging because most cases develop sporadically without inherited genetic mutations, and because of the gradual progression of symptoms over the course of disease. Recognizing affected individuals early would be important for increasing treatment options and facilitating clinical trials of new therapeutics. However, the currently available preclinical diagnostics based on amyloid peptide and tau protein forms in the cerebrospinal fluid are not sufficiently specific, as individuals exhibiting them may still retain normal cognitive capabilities for years before developing dementia.
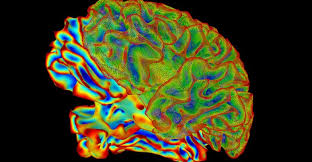
In the present work, the teams led by Michael Ewers (ISD) and EMBO Member Christian Haass (DZNE) focussed on the TREM2 protein, which functions in specialized brain immune cells called microglia that clear toxic material resulting from nerve cell injury. Microglia are activated during Alzheimer’s disease progression and may mediate an initially protective inflammatory response, a notion that is also supported by epidemiological studies linking mutations in the TREM2 gene to increased risk of Alzheimer’s and other neurodegenerative diseases. Conducting a cross-sectional study of a large cohort of patients with different levels of cognitive impairment and different disease stages, the researchers found that the amounts of a TREM2 fragment in the cerebrospinal fluid were highest during early stages characterized by mild cognitive impairment symptoms. Its levels declined again in late-stage patients with full dementia, closely mirroring the pattern of microglia activity during the course of the disease. Together, these findings indicate that microglia-mediated brain inflammation may demarcate the transition from preclinical Alzheimer’s disease to full dementia.
“We now have the first marker for the capacity of brain immune cells to remove toxic materials,” says Haass, “and its increase long before full Alzheimer’s dementia shows that there is early neuronal injury that does not yet affect memory, but already triggers a microglia response.” And Ewers adds, “If this response is indeed protective, then therapeutically modulating the activity of microglia could be beneficial in late-stage Alzheimer’s patients as well as other brain disorders.”