Multiple system atrophy (MSA), a neurodegenerative disorder resembling Parkinson’s disease, was first described in 1960, but the distinction between the causes of MSA and Parkinson’s remained murky. New research, however, indicates that MSA is caused by a unique prion. This prion appears to differ from the prion that is suspected of playing a role in Parkinson’s. It is, moreover, the first new prion to be associated with human disease in 50 years.
Fittingly, the new discovery is the work of a research team that includes Stanley Prusiner, M.D., the Nobel Prize winner who isolated the previously identified prion. This prion, which Dr. Prusiner first characterized in 1982, has been implicated in several related diseases scrapie in sheep; bovine spongiform encephalopathy, or “mad cow” disease, in cattle; and variant Creutzfeldt-Jakob disease in humans.
Prion researchers have since suggested that similar misfolded proteins may contribute to more common forms of neurodegeneration, such as Parkinson’s disease and Alzheimer’s disease.
“Now we’ve conclusively shown that a new type of prion causes MSA,” said Kurt Giles, D.Phil., a colleague of Dr. Prusiner’s and an associate professor of neurology at the University of California, San Francisco. “This is our mark in the sand.”
Dr. Giles is the senior author of a new research paper “Evidence for α-synuclein prions causing multiple system atrophy in humans with parkinsonism” that appeared August 31 in the Proceedings of the National Academy of Sciences.
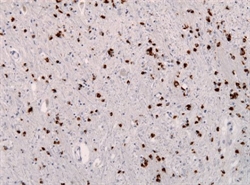
“To determine whether human α-synuclein forms prions, we examined 14 human brain homogenates for transmission to cultured human embryonic kidney (HEK) cells expressing full-length, mutant human α-synuclein fused to yellow fluorescent protein (α-syn140*A53T–YFP) and TgM83+/− mice expressing α-synuclein (A53T),” wrote the authors. “The TgM83+/− mice that were hemizygous for the mutant transgene did not develop spontaneous illness; in contrast, the TgM83+/+ mice that were homozygous developed neurological dysfunction.”
Essentially, the researchers established that mice exposed to human MSA tissue developed neurodegeneration. In addition, the team found that the brains of infected mice contained abnormally high levels of insoluble human α-synuclein, and that infected mouse brain tissue could itself spread the disease to other mice.
“All of the MSA extracts also induced aggregation of α-syn*A53T–YFP in cultured cells, whereas none of six Parkinson’s disease extracts or a control sample did so,” the authors continued. “Our findings argue that MSA is caused by a unique strain of α-synuclein prions, which is different from the putative prions causing PD and from those causing spontaneous neurodegeneration in TgM83+/+ mice.”
The discovery that alpha-synuclein prions can transmit MSA raises a public health concern about treatments and research that involve contact with brain tissue from neurodegeneration patients, because standard disinfection techniques that kill microbes do not eliminate the prions that cause Creutzfeldt-Jakob disease. Whether the same challenges hold for α-synuclein prions in MSA remains to be determined.
The authors warned that clinicians and researchers should adopt much more stringent safety protocols when dealing with tissue from patients with MSA and other neurodegenerative diseases, many of which they believe may also be caused by prions. For instance, MSA is frequently initially diagnosed as Parkinson’s disease, which is often treated with deep-brain stimulation. The disease could potentially be transmitted to other patients if deep-brain stimulation equipment is reused.
“You can’t kill a protein,” Dr. Giles said. “And it can stick tightly to stainless steel, even when the surgical instrument is cleaned.” As a result, he added, “We’re advocating a precautionary approach. People are living longer and likely getting more brain surgeries. There could be undiagnosed neurodegenerative diseases that if they’re caused by prions mean infection could be a real worry.”
Unlike the danger of bovine spongiform encephalopathy from contaminated beef, the researchers stress that there is no apparent risk of infection by MSA prions outside of specialized medical or research settings.