Highlights
- •SARS-CoV-2-infected human stem cell-derived lung and cardiac cells via ACE2
- •Responses to SARS-CoV-2 infection varied between lung and cardiac cells
- •Druggable kinases were identified via phosphoproteomics profiling of infected cells
- •Alectinib and SPHINX31 were both shown to inhibit viral replication in vitro
Summary
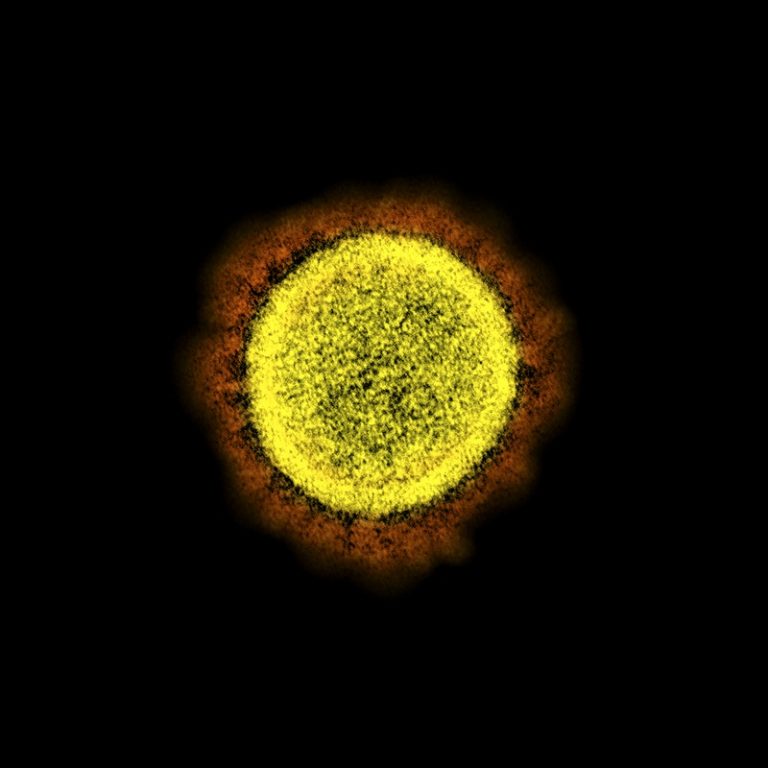
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily infects the respiratory tract, but pulmonary and cardiac complications occur in severe coronavirus disease 2019 (COVID-19). To elucidate molecular mechanisms in the lung and heart, we conducted paired experiments in human stem cell-derived lung alveolar type II (AT2) epithelial cell and cardiac cultures infected with SARS-CoV-2. With CRISPR-Cas9-mediated knockout of ACE2, we demonstrated that angiotensin-converting enzyme 2 (ACE2) was essential for SARS-CoV-2 infection of both cell types but that further processing in lung cells required TMPRSS2, while cardiac cells required the endosomal pathway. Host responses were significantly different; transcriptome profiling and phosphoproteomics responses depended strongly on the cell type. We identified several antiviral compounds with distinct antiviral and toxicity profiles in lung AT2 and cardiac cells, highlighting the importance of using several relevant cell types for evaluation of antiviral drugs. Our data provide new insights into rational drug combinations for effective treatment of a virus that affects multiple organ systems.
Introduction
Coronavirus disease 2019 (COVID-19) is primarily a respiratory disease, with 80% of infections clinically mild or asymptomatic. Progression to severe illness is associated with lower respiratory tract involvement (Chen et al., 2021b; Hou et al., 2020). In addition to pulmonary disease, cardiovascular, renal, digestive, and neurological complications are reported (Nalbandian et al., 2021). Cardiac complications include arrhythmias, thromboembolism, and acute myocardial injury (Lazzerini et al., 2022; Shi et al., 2020). Cardiac involvement is observed in up to 78% of recovered COVID-19 patients, and ongoing myocardial inflammation is observed in 60% of patients (Goyal et al., 2020; Puntmann et al., 2020). Furthermore, myocardial injury was associated with increased mortality (Shao et al., 2020). While cardiac damage during COVID-19 is predominantly thought to be due to an over-exuberant immune response, studies of autopsy tissue from patients who died from COVID-19 have detected viral RNA and spike (S) antigen in the heart (Deinhardt-Emmer et al., 2021; Schneider et al., 2020; Wang et al., 2021).
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mediates infection by binding of the S protein to its receptor, angiotensin-converting enzyme 2 (ACE2) (Zhou et al., 2020). The S protein is cleaved into two domains, S1 and S2, by host cell proteases (Shang et al., 2020). Following attachment, fusion with the cell membrane requires further proteolytic cleavage at the S2′ site to activate the fusion peptide (Hoffmann et al., 2020). This is mediated extracellularly by serine proteases including transmembrane protease, serine 2 (TMPRSS2) or in endosomes by cathepsin L (Hoffmann et al., 2020; Ou et al., 2020; Perez-Bermejo et al., 2021). Thus, ACE2 is a critical determinant of the tissue tropism of SARS-CoV-2, as is the presence of surface and/or endosomal proteases. ACE2 is expressed in many human tissues, with the highest ACE2 expression observed in the nasal epithelium, lungs, ileum, and heart (Hamming et al., 2004; Muus et al., 2021; Qi et al., 2020; Sungnak et al., 2020; Zou et al., 2020). Tissue sites containing cells that co-express ACE2 and TMPRSS2 include the nose, lungs, kidney, gastrointestinal tract, and the gallbladder (Muus et al., 2021; Sungnak et al., 2020), while cells co-expressing ACE2 and cathepsin L are found within the lung, heart, and gastrointestinal tract (Muus et al., 2021). Following entry, the virus interacts with cellular machinery to complete its replication cycle and triggers a host cell response that can vary in different organs.
We sought to elucidate the molecular mechanisms of SARS-CoV-2 infection in lung and heart using human stem cell-derived lung and cardiac cells. Human pluripotent stem cells (hPSCs) including both human embryonic stem cells (hESCs) and induced pluripotent stem cells (hiPSCs) have been used to generate functional human cells, tissues, and organoids to model human disease. We and others have generated stem cell-derived lung alveolar type II (AT2) epithelial cell and cardiac cultures that can be productively infected with SARS-CoV-2 (Huang et al., 2020; Perez-Bermejo et al., 2021; Sharma et al., 2020; Williams et al., 2021). We hypothesized that paired experiments in SARS-CoV-2-infected lung and cardiac cells would reveal important similarities and differences in viral and host factors that could inform treatment of COVID-19 and its complications. We used CRISPR-Cas9-mediated knockout of ACE2 and demonstrated that ACE2 was essential for SARS-CoV-2 infection of both cell types. Small-molecule inhibitors revealed distinct mechanisms of SARS-CoV-2 entry. We identified differential cellular responses to SARS-CoV-2 infection by transcriptome profiling and phosphoproteomics and further demonstrated the utility of these stem cell-derived models for screening antiviral compounds for anti-SARS-CoV-2 activity. Our findings provide new insights into treatment strategies for COVID-19.
Results
SARS-CoV-2 productively infects human stem cell-derived lung AT2 and cardiac cultures
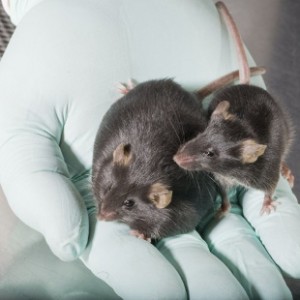
hESC- and iPSC-derived cardiomyocyte (Anderson et al., 2018; Lopes et al., 2021) and AT2 lung (Jacob et al., 2017) cultures were generated to develop in vitro models of SARS-CoV-2 infection (Figure 1A). Lung AT2 cultures expressed the AT2 cellular markers surfactant protein C (SFTPC) and HT2-280, along with the lung development homeobox protein NKX2-1 and an absence of aquaporin-5 (AQP5), FOXJ1, and SCGB3A2, confirming differentiation into AT2 cells (Figure S1A). Gene expression profiling of the lung AT2 and cardiac cells demonstrated transcriptional profiles consistent with high levels of AT2 cells and cardiomyocytes, respectively (Figures S1B and S1C).
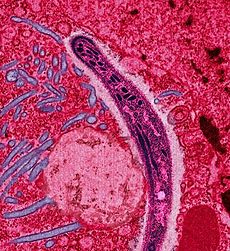
To determine susceptibility to SARS-CoV-2 infection, lung AT2, cardiac, and Vero cells were inoculated with the ancestral strain of SARS-CoV-2. As expected, SARS-CoV-2 productively infected Vero cells with virus titers and E gene copies peaking at 3 days post-infection (dpi) (Figure 1B). SARS-CoV-2 showed robust virus replication in AT2 cells, with virus titers and E gene copies peaking at 4 dpi (Figure 1B). Immunostaining for double-stranded RNA (dsRNA) showed evidence of SARS-CoV-2 replication at 3 dpi (Figure 1C). Cardiac cell cultures differentiated from hESCs (NKX2-5eGPF/w [Elliott et al., 2011]) were also susceptible to SARS-CoV-2 infection, with virus titers and E gene copies peaking slightly later than AT2 cells between 4 and 6 dpi (Figure 1B). Cardiac cells generated from ALPK3 knockout hESCs that model hypertrophic cardiomyopathy (Phelan et al., 2016), were similarly susceptible to SARS-CoV-2 infection, with a peak in virus titers at 4 dpi (Figure S1D). Immunostaining showed SARS-CoV-2 dsRNA in both cardiomyocyte and non-cardiomyocyte cells within the cardiac cultures (Figure 1C). Furthermore, cardiac cultures infected with SARS-CoV-2 stopped contracting at 4 dpi (Video S1). Overall, these data show that SARS-CoV-2 replicates efficiently in cardiac and lung AT2 cells, consistent with published reports (Huang et al., 2020; Perez-Bermejo et al., 2021)….