Abstract
Squamous cell carcinomas are triggered by marked elevation of RAS–MAPK signalling and progression from benign papilloma to invasive malignancy1,2,3,4. At tumour–stromal interfaces, a subset of tumour-initiating progenitors, the cancer stem cells, obtain increased resistance to chemotherapy and immunotherapy along this pathway5,6. The distribution and changes in cancer stem cells during progression from a benign state to invasive squamous cell carcinoma remain unclear. Here we show in mice that, after oncogenic RAS activation, cancer stem cells rewire their gene expression program and trigger self-propelling, aberrant signalling crosstalk with their tissue microenvironment that drives their malignant progression. The non-genetic, dynamic cascade of intercellular exchanges involves downstream pathways that are often mutated in advanced metastatic squamous cell carcinomas with high mutational burden7. Coupling our clonal skin HRASG12V mouse model with single-cell transcriptomics, chromatin landscaping, lentiviral reporters and lineage tracing, we show that aberrant crosstalk between cancer stem cells and their microenvironment triggers angiogenesis and TGFβ signalling, creating conditions that are conducive for hijacking leptin and leptin receptor signalling, which in turn launches downstream phosphoinositide 3-kinase (PI3K)–AKT–mTOR signalling during the benign-to-malignant transition. By functionally examining each step in this pathway, we reveal how dynamic temporal crosstalk with the microenvironment orchestrated by the stem cells profoundly fuels this path to malignancy. These insights suggest broad implications for cancer therapeutics.
Main
Squamous cell carcinomas (SCCs) are common life-threatening cancers of the stratified epithelia of skin, oral cavity, oesophagus and lungs1,8,9. Even for skin, where SCCs are often caught early, their frequency of occurrence and ever-rising metastatic incidences pose major health concerns10. Chemical carcinogenesis studies expose elevated RAS–MAPK signalling, often involving oncogenic Ras mutations, as critical in the path to invasive SCCs2,3,4. The lengthy delay and sporadic nature of mutagen-mediated SCCs has led to the view that additional oncogenic mutations are needed3,11,12,13, further supported by the high mutational burden associated with human metastatic SCCs7. However, genetically induced SCCs display many fewer mutations than mutagen-driven SCCs3,14, and skin tumours exhibiting a heterogeneous benign/SCC phenotype can be initiated even with HRASG12V alone6. These observations raise the possibility that non-genetic alterations may be potent cancer drivers.
Increasing evidence has highlighted extrinsic perturbations—for example, inflammation, metabolism and wounding—in preconditioning tissues to heightened cancer vulnerabilities6,14,15,16,17,18,19. It is less clear whether and how in healthy tissues an oncogenic mutation in a stem cell can intrinsically stimulate environmental changes that may lessen the need for multi-step mutagenesis. Here we address this issue using a single HRASG12V oncogene model that clonally activates a reliable path to aggressive, invasive cutaneous SCCs. After performing deep single-cell RNA sequencing (scRNA-seq) to gain insights into the SCC cancer stem cell (CSC) signature, we trace its temporal origins and physiological importance. We show that, after oncogenic RAS initiation, tissue stem cells begin an aberrant molecular dialogue with their surroundings, culminating in a considerable remodelling of the tumour microenvironment at the benign-to-malignant transition. This provides fertile ground for stromal TGFβ-mediated induction of leptin receptor (Lepr) and vasculature-mediated elevation of tissue leptin, leading to LEPR–leptin signalling and PI3K–AKT–mTOR in CSCs to drive the invasive switch. Triggered by oncogenic RAS, each step of this stem cell–microenvironment crosstalk cascade is essential for malignant progression, and it involves pathways that are often mutated in advanced SCCs with a high mutational burden.
Newfound heterogeneity in CSCs
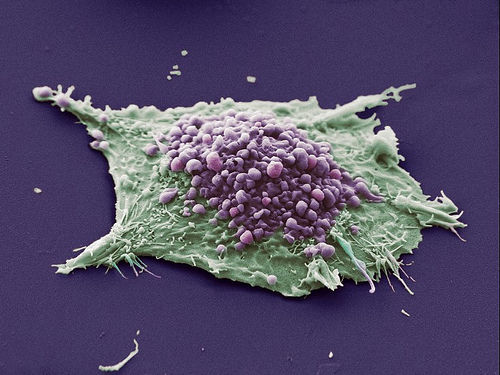
Skin stem cells that acquire HRAS mutations go through a benign papilloma state before progressing to malignant, invasive SCCs20,21. On the basis of serial transplantations, tumour-initiating CSCs from mouse SCCs are enriched for integrins and reside at tumour-stromal interfaces22,23. In tumours displaying a mixed phenotype, basal progenitors undergoing TGFβ signalling are enriched for CSCs with increased resistance to chemotherapy and immunotherapy, and the loss of TGFβ signalling reverts tumours to a benign state5,6,19.
To control tumorigenesis, we took embryonic day 9.5 (E9.5) FVB mouse embryos with a tetracycline-inducible RAS oncogene (TRE-HRASG12V) and performed low-titre in utero lentiviral delivery to selectively transduce a small number of skin basal progenitors with an rtTA3 transactivator and TGFβ reporter under the control of pSMAD2/3–SMAD4-complex-binding elements (SBE) (Fig. 1a). Postnatal doxycycline resulted in clonally transduced skin patches of activated HRAS(G12V). By around 4 weeks, hyperplastic, well-differentiated benign papillomas with smooth undulating epithelial–mesenchymal borders had formed, of which most advanced to undifferentiated, uniformly invasive SCCs by about 8 weeks (Fig. 1a). SCCs displayed only sparse differentiated keratin pearls, while most epithelial–stromal borders were poorly defined. As judged by immunofluorescence imaging and fluorescence-activated cell sorting (FACS), TGFβ signalling and the phosphorylation of its downstream target transcriptional cofactor SMAD2 (pSMAD2) were rare in papillomas but increased substantially in invasive SCC progenitors (Fig. 1b and Extended Data Fig. 1a,b). Taken together with our previous analysis of mixed papilloma–SCC tumours6, this result provided an important temporal layer by linking TGFβ signalling to the progression of CSCs from benign to malignant states…