When I visited Ricaurte, Colombia, in 2016, I was surrounded by men with long faces and prominent ears. As we spoke, they would ask repetitive questions while mumbling and failing to maintain eye contact, and when they shook my hand, they turned their body away from me. They were interested in me but were too shy to interact. This type of anxiety-related approach-withdrawal behavior is typical of those with fragile X syndrome (FXS), a well-characterized genetic disease that is the most common inherited form of intellectual disability and the most common single-gene cause of autism. Even many of the Ricaurte women, who usually have at least one good copy of the X chromosome, showed similar social deficits. I had never seen so many individuals with FXS all together. I thought to myself: This is ground zero for FXS.
Likely because the founding families of this small village had one or more carriers of the causative mutation, Ricaurte has the highest known prevalence of FXS in the world. Last year, our team published the results of genetic testing of almost all of the inhabitants in this village. We found that nearly 5 percent of male and more than 3 percent of female inhabitants of Ricaurte have FXS,1 compared to around 0.02 percent of people living in the US and in Europe. In Ricaurte, the residents are supportive of these individuals, who work in the community and are well accepted. Their behavior does not seem unusual to those living in the village. Relatives who have moved away from Ricaurte and then subsequently have had a child with FXS will move back to this town for the acceptance and support they find there. This pattern further enhances the genetic cluster of FXS-causing mutations in this area.
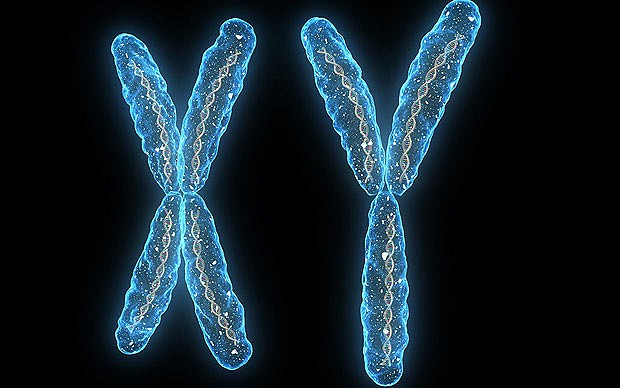
Initial chromosome testing documented the fragile site on the X chromosome, and we saw the disease’s high prevalence as an advantage in our quest to study the hard-to-treat condition. While research of the past three decades has detailed the underlying genetic and molecular causes of FXS, it has yet to yield a treatment that can reverse the associated neurobiological abnormalities in the brain. By analyzing the genomes of FXS patients in the village, we hope to learn more about the founders and to investigate the background allelic variations that facilitate the appearance of new FXS mutations. We are also investigating individual variability and whether environmental toxicity can exacerbate FXS patients’ conditions.
At the same time, we are conducting several controlled trials of promising FXS drug candidates at the MIND Institute at the University of California, Davis, Medical Center. The candidates include cannabidiol as well as metformin, a type 2 diabetes medication that can also help obesity. We are hopeful that our work in Ricaurte, along with the work of other teams investigating populations with high rates of FXS in Indonesia, Israel, and on the Spanish island of Mallorca, among other places, will inform the development of better treatments for patients all over the world.
What we know about fragile X
Fragile X syndrome was named for a delicate site at the bottom of the X chromosome of patients with the disease that for unknown reasons looked “fragile” when their cells were studied in culture media deficient of folic acid. In 1991, researchers identified an expansion of the DNA sequence CGG in the promoter region of the FMR1 gene as the underlying cause of the X chromosome’s broken appearance. This gene codes for fragile X mental retardation protein (FMRP), which controls the translation of hundreds of messenger RNAs into various proteins that are important for neuronal function. FMRP is the main controller of synaptic plasticity in early brain development and is needed throughout life to make new neurons. Recent research has found that the protein also controls a protein essential for epigenetic changes across the genome, perhaps explaining FMRP’s wide-ranging effects.
The mutated FMR1 gene itself harbors epigenetic differences. While the wildtype gene lacks methylation, sequences with more than 200 CGG repeats—considered the full mutation—are heavily methylated, which thereby blocks transcription of the gene. In males, this leads to a complete absence of FMRP, while females typically have one X with the wildtype gene that provides some amount of the protein. As a result, their symptoms are typically less severe.
Some individuals carry what is called the premutation, characterized by a CGG expansion of 55 to 200 repeats. Premutation genes with fewer than 120 CGG repeats typically result in normal FMRP levels, while those with more repeats have lowered FMRP production, leading to relatively minor learning problems or, rarely, intellectual disabilities. Up to a normal threshold, generally the more FMRP produced, the higher your IQ. Paradoxically, premutations result in higher FMR1 mRNA levels than are found in wildtype individuals, and these RNAs can cause problems even if FMRP protein levels are normal. (See “Sidebar” on page 51.)
If women carrying the premutation pass it on, it can expand into the full mutation during egg development. Once the CGG repeats number more than 100, every time that X chromosome is passed from mother to child it will carry the full mutation, as the CGG repeats apparently expand during either oogenesis or embryonic development. The details of this expansion are still murky. Male carriers of the premutation will pass it on to all of their daughters. If a man carries a full mutation, it reverts back to a premutation in his sperm, such that all of his daughters inherit the premutation. Again, the reason for and mechanisms of this back mutation are unclear. (See illustration on page 49.)
Despite questions about how the FXS locus shuffles CGG repeats in a somewhat predictable manner, the underlying molecular mechanisms of the disease are fairly well characterized, thanks to copious research on FMRP’s role in the cell. This has led to human trials of several treatments that target the relevant molecular pathways, but unfortunately, they’ve had little success. While there are therapies to manage symptoms, there is currently no cure for FXS.
Our failure in treatment trials
There are many ways to cure a mouse of FXS. For example, inhibitors of the metabotropic glutamate receptor 5 (mGluR5) pathway, which is involved in neural signaling and is known to be overactive in FXS, can relieve mouse models of all symptoms of the disease. But when such therapies moved into human trials a few years ago, adolescents and adults with FXS experienced no benefit beyond what the placebo group enjoyed. Similarly, agonists that target the neurosignaling GABA system, which is underactive in FXS, succeeded in alleviating symptoms in mice but in humans proved no better than placebo.2,3 Regardless of whether patients got the mGluR5 inhibitor, GABA agonist, or the placebo, between 20 percent and 30 percent of patients showed improved behavior and their families were feeling positive about the outcome.4,5
Given the high expectations among patients and their families for targeted FXS treatments, such high placebo responses are common. There is thus a need for quantitative outcomes that measure patient responses to treatment through electrophysiological measures. In the last six years, such measures have been developed. For example, event-related potentials (ERPs), patterns of activity visible on EEG readouts in response to sensory cues, can reveal the failure of FXS patients to habituate to repeated stimuli such as repetitive sounds or visual stimuli, leading to hyperarousal. Another option is to track patients’ eye movements to monitor their ability to make eye contact. There are also new molecular biomarkers that reflect a reversal of the neurobiological changes in FXS. For example, a protein called matrix metallopeptidase-9 (MMP-9) is elevated in the blood of FXS patients, and a targeted treatment such as metformin lowers the MMP-9 level in mice and patients with FXS.