Eggs and sperm do it when they combine to make an embryo. John Gurdon did it in the 1960s, when he used intestinal cells from tadpoles to generate genetically identical frogs. Ian Wilmut did it too, when he used an adult mammalian cell to make Dolly the sheep in 1996. Reprogramming reverting differentiated cells back to an embryonic state, with the extraordinary ability to create all the cells in the body has been going on for a very long time.
Scientific interest in reprogramming rocketed after 2006, when scientists showed that adult mouse cells could be reprogrammed by the introduction of just four genes, creating what they called induced pluripotent stem (iPS) cells1. The method was simple enough for almost any lab to attempt, and now it accounts for more than a thousand papers per year. The hope is that pluripotent cells could be used to repair damaged or diseased tissue something that moved closer to reality this year, when retinal cells derived from iPS cells were transplanted into a woman with eye disease, marking the first time that reprogrammed cells were transplanted into humans (see Naturehttp://doi.org/xhz; 2004).
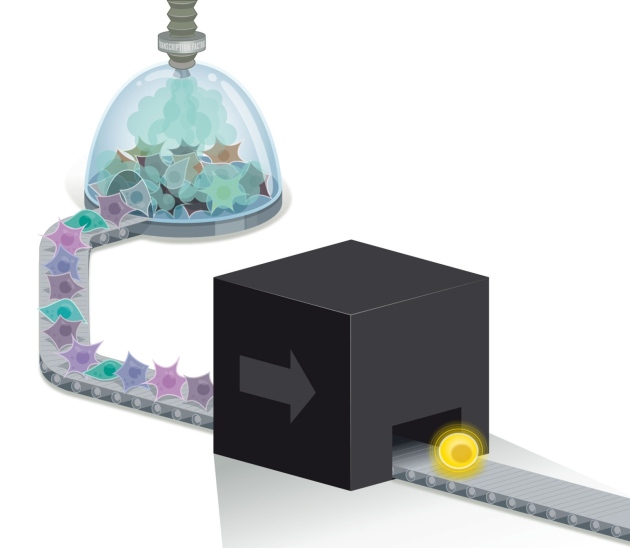
There is just one hitch. No one, not even the dozen or so groups of scientists who intensively study reprogramming, knows how it happens. They understand that differentiated cells go in, and pluripotent cells come out the other end, but what happens in between is one of biology’s impenetrable black boxes. “We’re throwing everything we’ve got at it,” says molecular biologist Knut Woltjen of the Center for iPS Cell Research and Application at Kyoto University in Japan. “It’s still a really confusing process. It’s very complicated, what we’re doing.”
One of the problems, stem-cell biologists say, is that their starting population contains a mix of cells, each in a slightly different molecular state. And the process for making iPS cells is currently inefficient and variable: only a tiny fraction end up fully reprogrammed and even these may differ from one another in subtle but important ways. What is more, the path to reprogramming may vary depending on the conditions under which cells are being grown, and from one lab to the next. This makes it difficult to compare experimental results, and it raises safety concerns should a mix of poorly characterized cells be used in the clinic.
But new techniques are starting to clarify the picture. By carrying out meticulous analyses of single cells and amassing reams of detailed molecular data, biologists are identifying a number of essential events that take place en route to a reprogrammed state. This week, the biggest such project an international collaboration audaciously called Project Grandiose unveiled its results2–6. The scientists involved used a battery of tests to take fine-scale snapshots of every stage of reprogramming and in the process, revealed an alternative state of pluripotency. “It was the first high-resolution analysis of change in cell state over time,” says Andras Nagy, a stem-cell biologist at Mount Sinai Hospital in Toronto, Canada, who led the project. “I’m not shy about saying grandiose.”
But there is more to do if scientists want to control the process well enough to generate therapeutic cells with ease. “Yes, we can make iPS cells and yes we can differentiate them, but I think we feel that we do not control them enough” says Jacob Hanna, a stem-cell biologist at the Weizmann Institute of Science in Rehovot, Israel. “Controlling cell behaviour at will is very cool. And the way to do it is to understand their molecular biology with great detail.”
Nuclear transfer
When Gurdon and Wilmut reprogrammed frog and sheep cells, respectively, they did it by transferring a differentiated nucleus into an egg stripped of its own DNA. Scientists knew that something in the egg was able to reprogram the nucleus, such that the genes associated with being a skin cell, for example, were switched off and those associated with pluripotency were switched on and triggered a cascade of downstream events. In the following decade, researchers found various new ways to reprogram adding nuclei to fertilized eggs and to embryonic stem cells but these methods did little to clarify what it was in the cells that did the reprogramming and how the process worked.
That changed when Shinya Yamanaka and Kazutoshi Takahashi at Kyoto University made iPS cells1. They showed that just four proteins that are usually expressed in early embryos or in embryonic stem cells could reprogram an adult cell and, crucially, they also provided a tool that researchers could use to study reprogramming in a culture dish, something they have been doing ever since. Stem-cell biologists now know that after introducing these proteins sometimes known as the Yamanaka factors there is a flurry of intense and mostly predictable gene expression. But then, after a few days, the cells enter a mysterious state in which they are dividing but stalled, failing to reprogram further. After a week or so, a slim few only one in a thousand become true pluripotent cells7……