Bacteria use two strategies to avoid being killed by antibiotics: resistance and tolerance. Resistance mechanisms such as destruction of a drug or modification of its target allow bacteria to grow in the presence of antibiotics. Tolerance is a property of dormant, nongrowing bacterial cells in which antibiotic targets are inactive, allowing bacteria to survive. The two phenomena are mechanistically distinct and assumed to be unrelated. On page 826 of this issue, Levin-Reisman et al. (1) show that tolerance nevertheless leads to resistance.
Bacteria acquire resistance through mutations or by acquiring foreign DNA (2). All resistance mechanisms ultimately prevent the antibiotic from binding to its target. Furthermore, bacteria can produce subpopulations of dormant (persister) cells that are tolerant to killing by existing antibiotics (3). The many mechanisms of persister formation include a drop in adenosine triphosphate (ATP) (4) and the activation of toxins that stop essential cellular processes (5). Persisters are particularly important in chronic infections (6). Antibiotic treatment selects for mutants that produce more tolerant cells (6, 7).
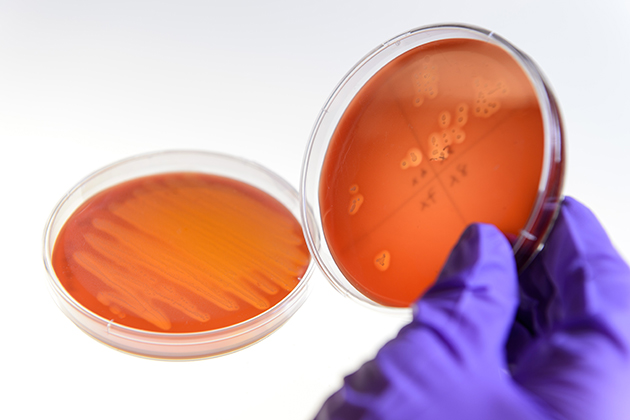
Levin-Reisman et al. now examine a possible link between tolerance and resistance. Members of the group previously found that mutants that take a long time to resume growth survive a lethal dose of ampicillin (8). In the new study, Levin-Reisman et al. inoculated stationary Escherichia coli cells into a fresh medium with a high dose of ampicillin. Most cells started to grow and were rapidly killed by the antibiotic (see the figure). The authors washed the few surviving cells and exposed them to subinhibitory levels of ampicillin, favoring selection of resistant mutants. The cells grew to stationary phase; after several cycles of killing by ampicillin and regrowth, resistant mutants emerged.
All mutants carried mutations in the promoter of the ampC gene, which encodes β-lactamase and is not expressed in wild-type E. coli, as well as mutations that increase tolerance. When the authors tracked the emergence of mutations over time, they found that tolerance precedes resistance (see the figure). Resistance developed faster if the starting strain carried a tolerance mutation. The results are particularly surprising given that the authors added ampicillin at a concentration that only allows growth of mutants with full resistance. Resistance to high levels of ampicillin requires two mutations in the ampC promoter.
Levin-Reisman et al.‘s experiment emulates antibiotic use in the clinic, where a high initial level is followed by diminishing amounts of the drug and several treatment cycles are applied. This produces conditions favorable to selection of tolerant mutants, which survive the initial antibiotic assault, allowing for the rise and survival of resistant cells (see the figure). Another reason for tolerance to precede resistance, as the authors note, is the vast difference between the mutation target size of the small ampC promoter and the many genes conferring tolerance.