Highlights
- •Tumor-treating fields (TTFs) do not affect natural killer (NK) cell viability
- •TTF exposure increased NK cell cytotoxic degranulation against GBM cells
- •TTFs had no effect on NK cell cytokine production
Summary
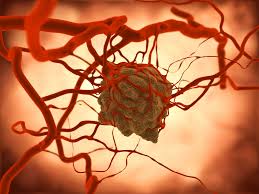
Tumor-treating fields (TTFs) are a non-invasive treatment for glioblastoma (GBM) that applies low-intensity, intermediate-frequency, alternating electric fields. Given a 5-year survival of less than 7% for GBM patients, multi-modal treatments are required to improve survival. Natural killer (NK) cells are innate lymphocytes that kill cancer cells and are thus a major target for new immunotherapy approaches. There is potential to combine TTFs with an NK cell-based therapy for GBM treatment. Here, we investigate the impact of TTFs on NK cell viability and functions. Exposure to TTFs does not affect NK cell viability or interferon (IFN)-γ production, a key NK cell function. Of significance, exposure to TTFs increases NK cell degranulation, a proxy of cell killing. These data suggest that the combination of TTFs and NK cell-based therapy may boost tumor cell killing. This provides a basis to further explore this combination, with the end goal of enhancing NK cell immunotherapy potential for patients with GBM.
Introduction
Tumor-treating fields (TTFs) are a non-invasive treatment that applies low-intensity, intermediate-frequency, alternating electric fields locally.1,2 These intermediate-frequency fields alternate too rapidly to induce stimulation of excitable tissue but do not cause excessive tissue heating.3 TTFs have a number of reported anti-cancer effects, including limiting cancer cell mitosis, decreasing cell invasiveness and the DNA repair response, and increasing cancer cell permeability to chemotherapy drugs.1,3 TTFs are generally used in the range of 100 to 300 kHz.1
In 2011, the FDA approved a TTF-based device for the treatment of glioblastoma (GBM), and it is now approved for primary and recurrent disease.4 GBM is an aggressive form of primary brain tumor that has a 5-year survival rate of less than 7%.5 Owing to its highly invasive nature, complete resection of the primary tumor is challenging, and thus, a multi-modal approach is often used and generally incorporates the chemotherapy temozolomide along with radiotherapy.6
Natural killer (NK) cells are innate lymphocytes that have potent cytotoxic and cytokine-producing functions.7,8 Peripheral blood NK cells can be broadly categorized into two subsets, each with unique functional specificities, namely CD56dim NK cells, which are highly cytotoxic, and the CD56bright subset, which produces the majority of NK cell-derived cytokines.8 NK cells can kill a variety of target cells, including tumor cells and virally infected cells, due to their ability to differentiate between normal and stressed cells. This places NK cells as central players in cancer immunosurveillance.8 NK cell recognition of target cells is balanced by the ligation of activating and inhibitory NK receptors with their ligands on target cells.7 GBM cell lines and primary cultures have been reported to express a host of activating and inhibitory NK cell ligands and would therefore be susceptible to NK cell-mediated cytotoxicity.9,10,11,12 NK cell infiltration and expression of related genes correlate with patient survival in GBM, indicating that the development of NK cell-based therapies for this poor-prognosis cancer is warranted.9,13,14 Indeed, as immunotherapy continues to cement itself as the fifth pillar of cancer treatment, NK cell-based immunotherapeutic approaches have gained considerable traction in recent years as an “off-the-shelf” alternative to T cell-based therapies.15,16,17 Already, an off-the-shelf NK cell-based therapy has shown significant promise for the treatment of GBM; however, it is likely that a multi-faceted approach will be required to elicit durable effects in patients.18 Indeed, the GBM tumor microenvironment is known to be immunosuppressive toward NK cells and hampers their efficacy within this environment. Previous studies have indicated dysfunctional NK cells within GBM lesions and highlighted multiple facets within this environment that can limit NK cell functionality.19,20,21 Therefore, identifying mechanisms to overcome this dysfunctionality and enhance the efficacy of autologous and allogeneic NK cell-based therapies is warranted.
There is limited information about the impact of TTFs on immune cells and how this non-invasive treatment may be combined with immunotherapeutic approaches.1,22,23,24 Here, for the first time, we sought to explore the impact of TTFs on NK cells and determine whether this treatment modality could be combined with an NK cell-based immunotherapeutic approach to boost efficacy in the harsh environment of GBM.
Results
Exposure to TTFs does not alter NK cell viability
Given that a variety of TTF mechanisms have been suggested for their anti-cancer cell activities, we first investigated the impact of TTFs on NK cell viability. Based on an understanding that while TTF devices for patients with GBM are worn for extended time periods, NK cell infusions into patients do not necessarily face similar exposure constraints, as they are prepared separately and can mediate rapid anti-tumor effects upon infusion25,26; we chose an 18-h exposure of NK cells to the TTF device as a useful starting point for these proof-of-principle experiments. Using primary NK cells from peripheral blood, there were no significant differences in the frequencies of live NK cells following exposure to 150, 200, or 250 kHz of TTFs for 18 h, as measured by flow cytometry (Figure 1A). Furthermore, there were no significant differences in the frequency of total NK cells within lymphocytes, nor the proportions of CD56dim and CD56bright functional subsets of NK cells, treated with and without a range of TTF treatments (Figures 1B and 1C)….