In a new landmark study, researchers from the University of North Carolina at Chapel Hill were able to convert skin cells into cancer-hunting stem cells that homed in and destroyed glioblastoma brain tumors. The investigators are optimistic that this technique could provide a significantly more effective treatment for the disease, which typically has a poor long-term survival rate.
“Patients desperately need a better standard of care,” remarked senior study author Shawn Hingtgen, Ph.D., assistant professor in the UNC Eshelman School of Pharmacy and member of the Lineberger Comprehensive Care Center.
The survival rate beyond two years for patients with a glioblastoma is only 30 percent due to its difficulty to treat. Moreover, even if surgical intervention removes the bulk of the tumor, it’s next to impossible to get the invasive, cancerous branches that spread deeper into the brain, which inevitably lead to regrowth. Sadly, most patients die within a year and a half of their diagnosis.
The investigators built upon previous Nobel Prize–winning research that allowed them to turn skin cells—specifically fibroblasts—into embryonic-like stem cells. Their goal was to develop a new personalized treatment for glioblastoma that starts with a patient’s own skin cells, with the aim of destroying the deep cancerous tendrils, effectively killing the glioblastoma.
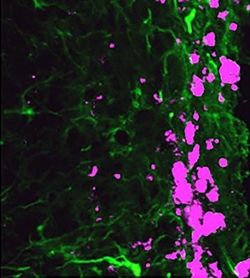
The UNC researchers were successful in reprogramming fibroblasts to become induced neural stem cells (iNSCs). Working with mice, the research team showed that the neural stem cells had the ability to move throughout the brain, home in on, and kill any remaining cancer cells. Additionally, the researchers demonstrated that these stem cells could be engineered to produce a tumor-killing protein, adding another blow to the cancer.
“We find that iNSCs genetically engineered with optical reporters and tumoricidal gene products retain the capacity to differentiate and induced apoptosis in co-cultured human glioblastoma cells,” the authors wrote. “Time-lapse imaging shows that iNSCs are tumoritropic, homing rapidly to co-cultured glioblastoma cells and migrating extensively to distant tumor foci in the murine brain.”
The findings from this study were published recently in Nature Communications through an article entitled “Therapeutically engineered induced neural stem cells are tumour-homing and inhibit progression of glioblastoma.”
Amazingly, depending on the type of tumor, the researchers were able to increase survival times in mice between 160 to 220 percent.
“Our work represents the newest evolution of the stem-cell technology that won the Nobel Prize in 2012,” Dr. Hingtgen explained. “We wanted to find out if these induced neural stem cells would home in on cancer cells and whether they could be used to deliver a therapeutic agent. This is the first time this direct reprogramming technology has been used to treat cancer.”
Dr. Hingten and his team are looking toward the next steps, which he said will focus on human stem cells and testing more effective anti-cancer drugs that can be loaded into the tumor-seeking neural stem cells.