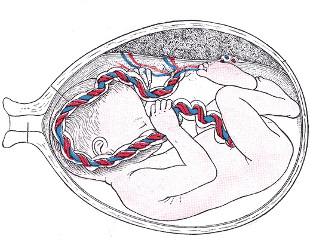
You’d think doctors and patients would be clamoring for cells so versatile they could help reboot a body suffering from everything from leukemia to diabetes. But a new report shows that an important source of these stem cells discarded umbilical cords is rarely utilized because of high costs and the risk of failure.
Stem cells drawn from the umbilical cord blood of newborn babies are sometimes used to treat medical conditions like lymphoma and sickle-cell anemia by replacing dysfunctional blood-producing cells in bone marrow. Yet less than 3 percent of cord blood collected in the United States is ever used, while the rest sit uselessly in blood banks, according to a September Genetic Engineering & Biotechnology News report.
“The cost of the cord is prohibitively high,” explained immunologist Enal Razvi, author of the report and director of Select Biosciences, a biotechnology consulting agency. Each unit of cord blood costs between $35,000 and $40,000, and most adults require two units for a successful transplant.
Unlike bone marrow, the main alternative stem cell source, cells transplanted from cord blood carry little risk of graft-versus-host disease, a deadly condition in which the body rejects a transplant. Scientists believe this is because a baby’s immune system is closer to a blank slate, so their stem cells can integrate with the patient’s body more easily. But cord blood transplants also take longer to start working, requiring longer hospital stays and upping the bill. Insurance companies will generally pay a set amount for a stem cell transplant regardless of where the cells come from. The price tag on a cord blood transplant can run up to $300,000, which may not be fully covered.
There is also a risk that a transplant could fail entirely, leaving patients with a compromised immune system in addition to their original disease and medical bills.
“It’s like spreading a small amount of seeds in a big garden,” said Mitchell Horwitz, who teaches cell therapy at Duke University Medical Center. “Sometimes it just doesn’t take.”
These complications help explain the low usage of cord blood in the United States. Razvi found that public cord blood banks, which store donated frozen units for transplants as needed, have only a 1 percent to 3 percent turnover annually. Most of their inventory sits unused year after year. For example, at Community Blood Services in New Jersey, patients have only used 278 of its 13,000 cords since it opened in 1996, according to business development director Misty Marchioni.
Usage is even lower at private cord blood banks, which charge clients thousands of dollars to store a cord in the event a family member one day needs it. Martin Smithmyer, chief executive of the private bank Americord said that most clients eventually use their cords, especially as more applications are found for cord blood-derived stem cells.
But some scientists disagree. Steven Joffe, who teaches medical ethics at the University of Pennsylvania Perelman School of Medicine said that many stem cell treatments can’t be done with a patient’s own stem cells since genetic diseases would already be present in the cord blood, and that bone marrow might be a better option for relatives.
“The likelihood they are ever going to use that product is vanishingly small,” he said.
Despite the low usage, advocates say cord blood programs have been crucial in improving transplant options for racial minorities, since it can be hard to find a bone marrow match for some groups. Cord blood doesn’t need to match the patient as closely as bone marrow.
“This has transformed the treatment of minority patients,” said Andromachi Scaradavou, the medical director at the National Cord Blood Program. “In the past, we didn’t have good donors to offer them.”
It is also a good emergency option, since finding a compatible bone marrow or peripheral blood donor can take months or years. “If you need a transplant quickly,” Marchioni said, “it’s easy to get cord blood off of a shelf.”
Still, experts are working on more efficient ways of ensuring widespread availability of cord blood without having so much of it sit forever unused. Each sample must be perfectly frozen in liquid nitrogen, so storage and maintenance for hundreds of thousands of unused cords gets expensive. This cost is at least partly transferred to the customers, according to Joffe, which increases the cost barrier for patients.
This isn’t an issue in all countries, however. In Japan, for example, 50 percent of transplants of this type use cord blood as the cell source, which possibly reflects the government’s pro-cord blood policies, said Scardavou.
Researchers are also continuing to look for ways to improve transplant success and to increase the number of stem cells obtained from each cord, potentially bringing down costs and making cord blood transplants feasible for more patients. “If the cost could be lowered,” said Scaradavou, “it would help a lot of patients get the treatment they need.”