Abstract
We aimed to identify markers in blood (serum) to predict clinically relevant knee osteoarthritis (OA) progression defined as the combination of both joint structure and pain worsening over 48 months. A set of 15 serum proteomic markers corresponding to 13 total proteins reached an area under the receiver operating characteristic curve (AUC) of 73% for distinguishing progressors from nonprogressors in a cohort of 596 individuals with knee OA. Prediction based on these blood markers was far better than traditional prediction based on baseline structural OA and pain severity (59%) or the current “best-in-class” biomarker for predicting OA progression, urinary carboxyl-terminal cross-linked telopeptide of type II collagen (58%). The generalizability of the marker set was confirmed in a second cohort of 86 individuals that yielded an AUC of 70% for distinguishing joint structural progressors. Blood is a readily accessible biospecimen whose analysis for these biomarkers could facilitate identification of individuals for clinical trial enrollment and those most in need of treatment.
INTRODUCTION
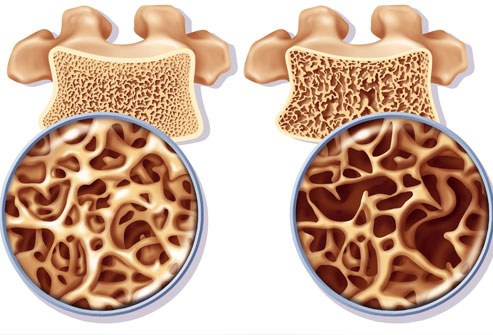
Osteoarthritis (OA), the most common joint disease, is a leading cause of disability in the United States and worldwide (1). A cure for OA remains elusive, and its management is largely palliative. This is mainly due to two major obstacles: inability to detect OA sufficiently early, before the onset of irreversible signs and recalcitrant symptoms; and inability to reliably identify individuals at high risk of OA progression, resulting in a high type II error rate, i.e., false-negative OA trials, due to inability to observe a treatment effect on a structural OA end point, such as a knee x-ray, that can only worsen but not improve in a cohort whose structural OA is relatively stable. Measures traditionally used to predict OA progression, such as age, sex, body mass index (BMI), and radiographic severity of OA, are minimally prognostic of structural worsening (2–4). The use of biomarkers in drug development increases by threefold the chance of successfully transitioning a drug from phase 1 to U.S. Food and Drug Administration approval (from 8 to 26%) (5). Thus, there is a strong need to identify OA biomarkers, particularly prognostic biomarkers, to facilitate means of identifying individuals likely to have OA progression during the study period and thereby enhance the success of OA clinical trials to bring to fruition the dream of disease modifying drugs for clinical use in OA.
Currently, however, available OA-related biomarkers are for research use only, and there are no blood-based biomarkers that are strongly predictive of OA progression. Moreover, the “chicken-and-egg” dilemma currently challenges the field; biomarkers are needed to enhance the success of trials, but qualification of biomarkers within successful trials is required to identify the best tools for differentiating specific disease phenotypes and potential responders to a treatment. Therefore, it is of great importance to be able to qualify biomarkers in the context of specific and clear phenotypes. In this work, we focus on the important unmet need of objectively identifying individuals at high risk of knee OA progression based on a user-friendly biospecimen, blood (serum), readily obtained in a clinical or trial setting.
Using a systematic, unbiased, and iterative approach based on extensive discovery proteomic studies in synovial fluid, urine, and serum from knee OA radiographic progressors and nonprogressors, we created a targeted multiple reaction monitoring (MRM) proteomic panel to predict radiographic knee OA progression by ultraperformance liquid chromatography–tandem mass spectrometry (UPLC-MS/MS) MRM analysis of serum samples (6). Our primary goal in this study was to evaluate the capability of this serum panel to predict clinically relevant knee OA progression (radiographic and pain worsening). We applied this MRM proteomic biomarker panel to the prediction of knee OA progression in the Foundation for the National Institutes of Health (FNIH) cohort, with further validation in the Biomarker Factory (BMF) cohort. The FNIH cohort was profiled previously for 18 commercially available enzyme-linked immunosorbent assay–based biomarkers (11 serum and 7 urinary) that were originally selected on the basis of existing evidence for their ability to predict OA progression (7, 8). Among these, urinary C-terminal cross-linked telopeptide of type II collagen (uCTXII) was the strongest prognostic biomarker of clinically relevant OA progression (8); uCTXII thereby provided a “best-in-class” reference against which we could evaluate the performance of our final serum proteomic biomarker sets. Through evaluation of their gene expression patterns in human knee OA articular chondrocytes and synoviocytes, we also explored the potential joint tissue origins of the serum proteomic biomarkers that were selected for inclusion in the final predictive biomarker sets.
RESULTS
FNIH cohort
In total, we quantitatively measured 177 peptides (101 proteins); the final analyses consisted of 107 peptides from 64 proteins that passed the quality control (QC) measures (table S1). We excluded a total of four samples: One was exhausted in laboratory preparation, two were outliers, and one had a missing data rate above 15%; this resulted in 596 FNIH study participants in the final analysis dataset with a mean age of 61.6 ± 8.9 years, a mean BMI of 30.7 ± 4.8 kg/m2, and 58.7% female (Fig. 1). At baseline, most participants had moderate to severe radiographic knee OA based on Kellgren-Lawrence (K/L) grades, mean medial minimum joint space width (JSW) reflecting degree of cartilage loss, and mean Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scores (Table 1). Most participants (70.5%) had no previous history of pain medication use. We defined four OA progressor groups based on the changes from baseline of radiographic joint space loss (JSL), which reflects cartilage degeneration, and/or WOMAC pain scores, resulting in 192 JSL and pain progressors, 103 JSL-only progressors, 102 pain-only progressors, and 199 JSL and pain nonprogressors (Table 1).