Many newly developed, potent cancer therapies aim to harness an immune response to target tumours1. However, a common problem with such immunotherapy approaches is the development of a severe inflammatory response called a cytokine storm2,3, in which levels of proteins called cytokines become abnormally high. This results in fever, low blood pressure, heart problems and, in some cases, organ failure and death. There is therefore great interest in understanding the underlying mechanisms to develop ways of preventing cytokine storms without altering the effectiveness of anticancer treatments. Writing in Nature, Staedtke et al.4 reveal that the protein ANP can block cytokine storms, and they uncover a self-amplifying production loop in immune cells that generates a class of molecule called catecholamines, which includes the hormone adrenaline (also known as epinephrine). They report that this catecholamine production helps to initiate and maintain cytokine storms.
When immune cells recognize a molecule that indicates a possible threat, they release cytokines that promote inflammation and orchestrate host defence5. One antitumour treatment that can trigger a cytokine storm uses a bacterium called Clostridium novyi-NT, which tracks to the low-oxygen environments found in certain tumours and releases spores that cause tumour-cell death6. Determining the correct bacterial dosage is difficult, and mice that have large tumours and receive a high dose of C. novyi-NT often develop a fatal cytokine storm that cannot be prevented by using inhibitor molecules to block the actions of cytokines or their receptors6.
To determine whether some known anti-inflammatory proteins could block a cytokine storm, Staedtke and colleagues engineered C. novyi-NT to secrete anti-inflammatory proteins and tested whether any of these bacteria could treat tumours effectively without causing severe toxicity owing to high cytokine levels. Their experiments revealed that ANP can dampen a cytokine storm. Mice treated with ANP-expressing C. novyi-NT had lower levels of proinflammatory molecules, including cytokines, in their bloodstream, and lower levels of organ infiltration by immune cells called myeloid cells that are associated with a cytokine storm, compared with mice given C. novyi-NT that had not been engineered to express ANP.
To determine how ANP decreased cytokine storms in their model system, Staedtke and colleagues characterized the differences between mice treated with the ANP-expressing C. novyi-NT and those that received non-engineered bacteria. This revealed that the dampened immune response linked to ANP was accompanied by a decrease in the level of catecholamines in the animals’ bloodstream. Catecholamines such as adrenaline are best known for their role as part of the ‘fight or flight’ response to acute stress, in which they are released by certain neurons and by the adrenal gland. The idea that catecholamines might act to promote cytokine storms seems counter-intuitive, given that molecules of this class are used routinely to treat the low blood pressure associated with cytokine storms. However, it was known7 that two types of immune cell — macrophages and neutrophils — produce catecholamines in response to inflammatory stimuli such as the molecule lipopolysaccharide (LPS), which is a hallmark of many types of bacterial infection.
To investigate whether catecholamines might have a key role in driving strong inflammatory responses, Staedtke et al. gave mice LPS and also gave a subset of these animals adrenaline. The animals that received adrenaline and LPS had higher cytokine levels and mortality than did those that received only LPS. Conversely, when the authors gave LPS to mice whose macrophages had been engineered to lack an enzyme called tyrosine hydroxylase (which is needed to make catecholamines), the animals had better survival rates and lower levels of cytokines and catecholamines than did LPS-treated mice that had macrophages with intact tyrosine hydroxylase. When the authors treated mice with a drug that blocks a receptor for catecholamines called the α1 adrenergic receptor, this interference with catecholamine signalling reduced inflammation when the mice were treated with LPS, compared with LPS-treated mice that did not receive the drug.
The authors also demonstrated the importance of catecholamines in initiating cytokine storms induced by bacteria in a different model system of severe bacterial infection. In both settings, the authors found that animals given metyrosine, a drug that inhibits tyrosine hydroxylase, had lower catecholamine and cytokine levels and increased survival rates compared with mice that did not receive the inhibitor.
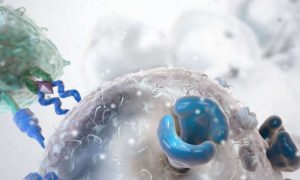
The next key question was whether catecholamine release has a function in cytokine storms that arise from immune-cell activation for reasons other than encounters with a bacterium. Immune cells called T cells that have been triggered to launch an immune response can also make catecholamines8. Certain immunotherapy approaches aim to generate such activated T cells by the administration of antibodies that can activate T cells or by the introduction of engineered T cells (called chimaeric antigen receptor (CAR) T cells) designed to target tumour cells. These approaches can cause a cytokine storm9,10. To test whether catecholamines might have a role in such cytokine storms, the authors administered a T-cell-activating antibody to a group of mice, and treated a subset of the mice with metyrosine. The animals that received the inhibitor had improved survival and lower cytokine levels than the mice that did not receive metyrosine.
The authors then studied human CAR-T cells that were grown in vitro together with the type of blood cancer cells that activate them. The medium from these cell cultures contained catecholamines and cytokines, and the levels of these molecules increased if adrenaline was added to the culture, providing support for a model of a self-amplifying response driving their production.
The authors went on to give CAR-T cells to mice carrying tumours. A subset of the mice were given ANP or metyrosine before receiving the CAR-T cells, and these animals’ cytokine levels were lower than were those of the mice that received only CAR-T cells. However, this difference did not affect the efficiency of the antitumour treatment, suggesting that toxicity due to cytokines is independent of the antitumour effects of this treatment.
Staedtke and colleagues provide compelling evidence for a self-amplifying circuit of catecholamine release by immune cells in the initiation of a cytokine storm (Fig. 1). However, determining the details of this circuitry will require additional studies. For example, how immune-cell activation drives an increase in catecholamine levels and how catecholamines boost cytokine production is unknown and should be investigated. Another mystery is which types of adrenergic receptor are crucial for the effects of catecholamines on cytokine levels in humans. ANP has anti-inflammatory properties11, but how it inhibits catecholamine production is another key unanswered question that deserves future study.