In carcinomas, cancer cells often win the loyalty of neighboring cells, stromal cells, that should know better. Rather than stand aside and let the immune system eliminate the cancer cells, credulous stromal cells, or connective tissue cells, interfere. They shield the cancer from the immune system and supply it with growth factors and nutrients. Even if cancer cells are subjected to a robust immune response, duped stromal cells can ensure that enough cancer cells survive to stage a cancer’s resurgence.
A way around this difficulty in treating cancer may seem obvious, if ruthless: kill the cancer cells and the duped cells. But there’s a problem: it’s hard to kill duped stromal cells without also killing wiser, more sensible stromal cells throughout the body. A potential solution, however, has been suggested by scientists based at the University of Oxford.
According to these scientists, who were led by Oxford oncologist Kerry D. Fisher, Ph.D., a vaccine already in clinical trials as a cancer killer can be modified so that it also causes cancer cells to betray their protectors. That is, the cancer cells are induced to take their friendly stromal cells down with them.
How? The vaccine, an oncolytic virus called enadenotucirev, causes cancer cells to produce a protein called a bispecific T-cell engager (BiTE). The BiTE is designed to bind to two types of cells and stick them together. In this case, one end is targeted to bind to fibroblasts. The other end specifically sticks to T cells, a type of immune cell that is responsible for killing defective cells. This triggers the T cells to kill the attached fibroblasts.
Details of this new immunotherapy approach appeared November 18 in the journal Cancer Research, in an article titled, “An Oncolytic Virus Expressing a T-cell Engager Simultaneously Targets Cancer and Immunosuppressive Stromal Cells.” The article describes how Dr. Fisher’s team caused cancer cells to produce a BiTE that not only binds to fibroblast activation protein on cancer-associated fibroblasts (CAF), but also to CD3ε on T cells, leading to potent T-cell activation and fibroblast death.
“Treatment of fresh clinical biopsies, including malignant ascites and solid prostate cancer tissue, with FAP-BiTE–encoding virus-induced activation of tumor-infiltrating PD1+ T cells to kill CAFs,” the article’s authors indicated. “In ascites, this led to depletion of CAF-associated immunosuppressive factors, upregulation of proinflammatory cytokines, and increased gene expression of markers of antigen presentation, T-cell function, and trafficking. M2-like ascites macrophages exhibited a proinflammatory repolarization, indicating spectrum-wide alteration of the tumor microenvironment.”
“We hijacked the virus’s machinery so the T-cell engager would be made only in infected cancer cells and nowhere else in the body,” noted Oxford’s Joshua D. Freedman, Ph.D., first author on the study. “The T-cell engager molecule is so powerful that it can activate immune cells inside the tumor, which are being suppressed by the cancer, to attack the fibroblasts.”
“Our new technique to simultaneously target the fibroblasts while killing cancer cells with the virus could be an important step towards reducing immune system suppression within carcinomas and should kick-start the normal immune process,” added Dr. Fisher. “These viruses are already undergoing trials in people, so we hope our modified virus will be moving towards clinical trials as early as next year to find out if it is safe and effective in people with cancer.”
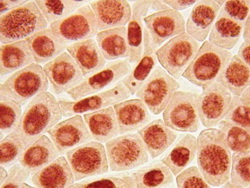
The scientists successfully tested the therapy on fresh human cancer samples collected from consenting patients, including solid prostate cancer tumors which reflect the complex make-up of real tumors. They also tested the virus on samples of healthy human bone marrow and found it did not cause toxicity or inappropriate T-cell activation.
The virus targets carcinomas, which are the most common type of cancer and start in cells in the skin or in tissues that line or cover internal organs, such as the pancreas, colon, lungs, breasts, ovaries, and prostate.