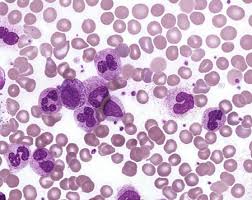
Chronic myelogenous leukemia (CML) is caused by chromosomal translocation that creates a fused gene; this gene produces an oncoprotein, BCR-ABL. Targeting this protein with imatinib (Gleevec) and other tyrosine kinase inhibitors (TKIs) produces dramatic clinical improvement in many patients ― but few cures. Many experts believe that cures are prevented because dormant (nonreplicating) cancer stem cells are not killed by TKIs and thereby sustain disease.
A French team reports that a molecular pathway, triggered by activation of peroxisome proliferator-activated receptor gamma (PPARγ), causes fewer cancer stem cells to remain dormant, thereby rendering them more vulnerable to treatment. The team added the PPARγ-activating drug pioglitazone, which is approved for diabetes, to imatinib in three patients with CML who had responded to imatinib but who had not achieved complete molecular responses (eradication of BCR-ABL transcripts). Each patient had a complete molecular response that has lasted as long as 4.7 years. In a nonrandomized phase II trial (ACTIM; still in progress), the authors report preliminary results showing that 57% of patients have achieved complete molecular responses so far.