Abstract
Despite many significant advances in 3D cell printing for skin, a disease model displaying the pathological processes present in the native skin has not been reported yet. Therefore, we were motivated for modeling a 3D diseased skin tissue with pathophysiological hallmarks of type 2 diabetes in vitro based on 3D cell printing technique. By stimulating epidermal-dermal intercellular crosstalk found in the native skin, it was hypothesized that normal keratinocytes would be differentiated as diabetic epidermis when interacting with the diabetic dermal compartment. To prove this, a novel wounded skin model was successfully devised during tissue maturation in vitro. Interestingly, the slow re-epithelization was observed in our diabetic model, which is a representative hallmark of diabetic skin. Using the versatility of 3D cell printing, the structural similarities and diabetic properties of the model were further augmented by addition of perfusable vascularized diabetic hypodermis. Insulin resistance, adipocyte hypertrophy, inflammatory reactions, and vascular dysfunction, as the typical hallmarks in diabetes, were found under hyperglycemia. Finally, the feasibility of this new disease model for drug development was successfully demonstrated through application of test drugs. We trust that this study provides a pioneering step towards 3D cell printing-based in vitro skin disease modeling.
Introduction
Skin health problems are often the first visible signs of diabetes according to the American Diabetes Association [1]. Type 2 diabetes can make existing skin problems worse and cause new troubles, such as diabetic dermopathy, diabetic blister, diabetic rash, fungal infections, and skin itching [1]. This issue happens when the body either does not respond normally to insulin or does not produce enough insulin to maintain a normal blood sugar level [2]. In particular, long-term diabetes complications with hyperglycemia (high blood glucose) tend to be associated with poor blood circulation. The reduced blood circulation into skin can impair cellular functions, such as proliferation, differentiation, and the secretion of extracellular matrix (ECM), which eventually makes self-healing difficult [3]. Because of the delay in wound healing, diabetic patients with damaged skin can develop an ulcer at high risk of an infection [3]. In this regard, 14%–24% of the patients would require an amputation, 85% of that is initiated on the bottom of the foot (called as diabetic foot ulcer) [3]. Despite this seriousness, it was reported that the diabetes-related skin diseases still have poor effective cure. The best way of the treatment was proposed as the prevention of its development in the first place and the change of lifestyle [4]. However, since many patients with foot ulcers have lost the ability to feel pain, it is difficult to notice the symptoms in the first place. After all, the primary goal in the treatment is to let the skin functions back to the normal conditions as effective as and as soon as possible with application of medications able to manage the blood glucose level and accelerate wound healing [5].
Previous studies mainly focused on development of diabetic animal models to investigate pathophysiology of skin response and develop medications for wound healing [[6], [7], [8]]. However, there were ethical concerns in using animal models and inaccurate in prediction because of the genetic discrepancy between human and animal are inevitable [9]. To overcome these limitations, engineering human skin models in vitro has recently been under attention as they can offer more accurate prediction in combination with primary human skin cells (fibroblasts, keratinocytes, and melanocytes) [10,11]. Indeed, 3D cell printing is a core technology for engineering highly vascularized heterogeneous skin layers (hypodermis, dermis, and epidermis) by enabling the precise deposition of various skin cells and biomaterials onto pre-defined positions [9]. In a pioneering work, droplets-based cell printing technique was applied to fabricate human skin fibroblasts and keratinocytes [12]. This technique enabled the sophisticated fabrication of multilayered skin construct using collagen type I as a bioink. That droplets-based printing incorporated melanocytes into an epidermal layer was used to enhance the rudimentary feature of skin [11]. The laser-induced forward transfer technique was also used to produce collagen tissue blocks including keratinocytes and fibroblasts [13]. In parallel to such technological advances, many bioinks were developed to better provide relevant microenvironments of skin [14]. Our research group also formulated a skin-derived bioink and demonstrated the material superiorities through in vitro and in vivo evaluations [13]. Collectively, 3D cell printing technique has been gaining momentum in modeling more realistic, predictive, and repetitive skin tissues [9].
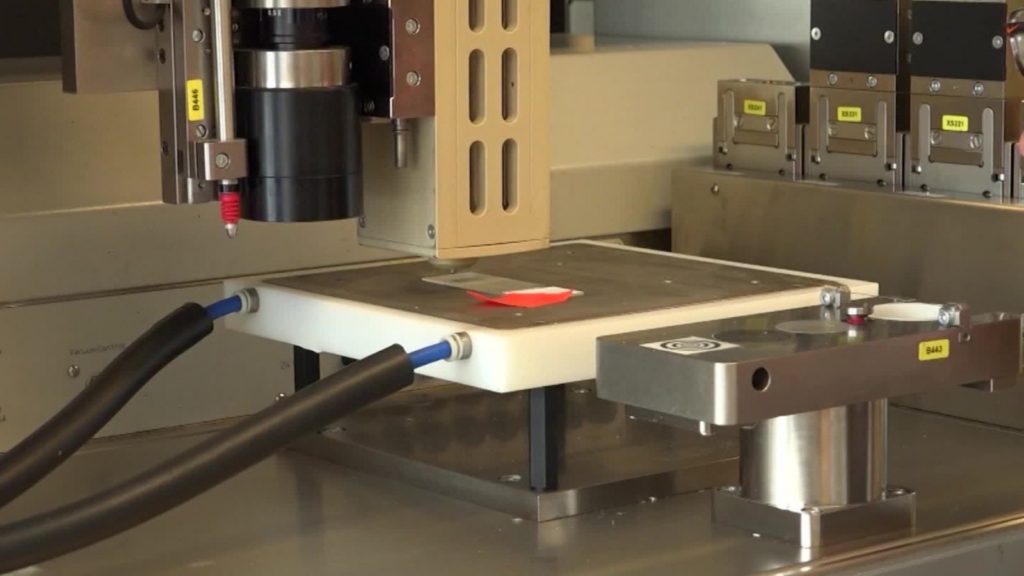
In spite of many outcomes, 3D cell printing in vitro diseased models have not been studied so far. Therefore, we were encouraged to model a diseased human skin with the clear properties of type 2 diabetes through 3D cell printing of the main skin layers (epidermis, dermis, hypodermis, and blood vessels) and utilization of the physiological phenomenon found in native skin. Fig. 1 shows some of the highlights of this study and the workflows. To overcome the issue of the poor differentiation potency of diabetic keratinocytes, we used the impact of epidermal-dermal crosstalk found in the native skin [[15], [16], [17]]. It was hypothesized that a diabetic human dermal fibroblasts (dHDFs)-loaded dermal layer could guide normal human epidermal keratinocytes (nHEKs) to be diabetic while forming matured epidermal layers. It would eventually lead to the development of mature diabetic full-thickness (epidermis/dermis) skin model. To prove this hypothesis, the stratified epidermal layers grown on dHDFs-loaded dermis were detached from the model and analyzed in views of histology and gene expression. More importantly, the wounded skin model fabricated using 3D cell printing was for the first time revised by incorporating printable polycaprolactone (PCL) to function as a 3D transwell system. The delayed re-epithelialization, which is a key feature of diabetic skin, was observed in the diabetic skin model. To further boost structural similarities and diabetic properties, we added hypodermal layer containing diabetic human preadipocytes (dHPAs) and perfusable vascular channel underneath the dermal layer, all in the printing process. Interestingly, the increased insulin resistance, vascular dysfunction, adipose hypertrophy, and pro-inflammatory responses, all typical hallmarks in diabetes, were found in our diabetic skin model. Finally, to demonstrate the potential applications of the engineered diabetic skin in dermatological studies and for drug testing, we applied the test drugs into the vascular channel for 3 days. The functional restorability of the epidermis and the reduced inflammatory response were accordingly observed.