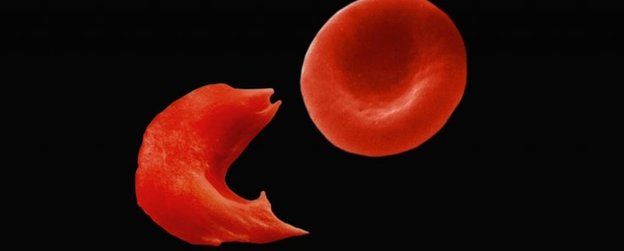
The substitution of valine for glutamic acid in the β-chain of hemoglobin S (HbS) is associated with the formation of hemoglobin polymers that promote vaso-occlusion, organ infarcts, and sickle cell crises. Polymer formation is retarded by hydroxyurea, which increases fetal hemoglobin, or by replacement of hematopoietic stem cells via allogeneic transplantation. But these measures are occasionally ineffective or infeasible in many patients with sickle cell disease (SCD). Replacement of the gene for βS-globin might cure this disorder.
To examine the safety and effectiveness of gene therapy for SCD, investigators prepared a modified βA-globin gene encoding an antisickling variant (βA-T87Q) incorporated into a self-inactivating lentiviral vector. The final product, LentiGlobin BB305, was transduced into bone marrow-enriched CD34+ cells obtained from a 13-year-old boy with severe homozygous SCD refractory to hydroxyurea. Following marrow ablation with busulfan, the patient was infused with the transduced stem cells.
Engraftment of neutrophils was achieved on day 38 after transplantation, and platelet engraftment was achieved on day 91. Various cell lines displayed progressive increases in gene marking, and hemoglobin rose to 12 g/dL, enabling red cell transfusions to be discontinued by day 88. By month 15 after transplantation, HbT87Q constituted 48% of hemoglobin, and HbS constituted 49%. Previous signs of hemolysis had disappeared, and no new SCD-related clinical events occurred. In addition, no evidence of lentivirus replication or insertional mutagenesis was observed.