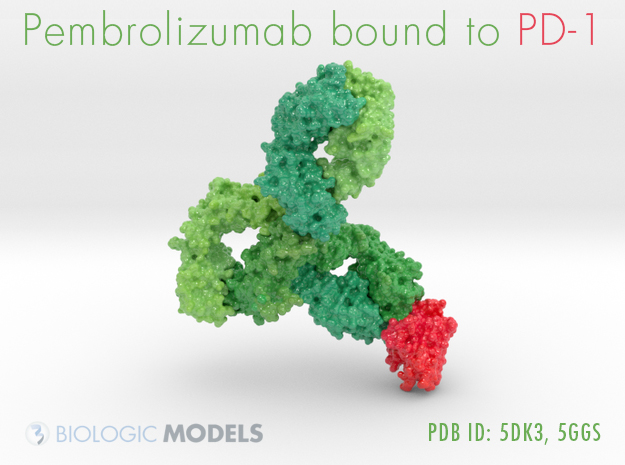
T cells eliminate pathogens by recognizing foreign proteins that are expressed on the cell surface (antigens). T cell activation in response to antigen occurs for a controlled period of time and is stopped by the expression of immune checkpoint proteins (1). Allison and colleagues proposed that antibody blockade of these proteins would enable prolonged T cell responses against cancer cells (2). The preclinical and clinical data that emerged using antibodies against two immune checkpoint proteins, cytotoxic T lymphocyte-associated protein 4 (CTLA4) and programmed cell death receptor-1 (PD-1), led to a paradigm shift in oncology as the treatment of some patients with these drugs led to tumor regression and durable survival for more than a decade (3). But as more patients with various types of cancer have been treated with immune checkpoint therapies, an enduring problem is to identify which patients are likely to respond. On page 409 of this issue, Le et al. (4) report the response to anti-PD-1 therapy (pembrolizumab) in 12 different tumor types, and show that patients who responded to the agent had defects in a DNA damage response pathway called mismatch repair.