Genetically modified viruses have successfully treated an antibiotic-resistant infection in a teenage girl, saving her life, researchers report today (May 8) in Nature Medicine. While this approach using engineered phages—viruses that infect bacteria—has only been tested in one person, the technique could be developed to battle other persistent, “superbug” infections.
“This is actually a historic moment,” Steffanie Strathdee, a professor of medicine at the University of California, San Diego, who was not involved in the study, tells NPR. “This is the first time that a genetically engineered phage has been used to successfully treat a superbug infection in a human being.” Strathdee says. “It’s terribly exciting.”
In the study, a teenager from England was suffering from an infection with a strain of Mycobacterium, a relative of the bacterium that causes tuberculosis. The girl had cystic fibrosis (CF) and had been on antibiotics to control bacterial infections that cause complications related to the genetic condition. She then endured a double lung transplant to treat the disease. Afterward, one of the infections spread throughout her body, and there weren’t any antibiotics that could treat it. At that point, Graham Hatfull, a professor of biotechnology at the University of Pittsburgh, got involved. He’d been working with phages, collecting them from the environment. He started to analyze his collection to see if any could kill the bacteria causing the patient’s infection.
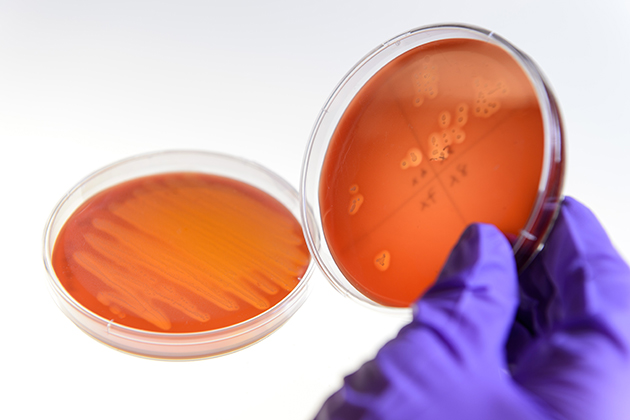
“The idea is to use bacteriophages as antibiotics—as something we could use to kill bacteria that cause infection,” Hatfull says in a Howard Hughes Medical Institute press release. His team identified three phages that appeared promising. One could infect and kill the bacterial strain making the patient sick. The other two weren’t as effective, so Hatfull and his colleagues tweaked the phages’ genomes, removing a gene, so the phages would kill the bacteria.
The team concocted a phage cocktail with all three viruses and tested it for safety on the patient’s skin. The cocktail was then given to the teen via IV. Several weeks later, a scan of her liver showed a significant drop in signs of infection, and it didn’t seem that the bacterial strain causing the infection was developing a resistance to the phage cocktail. Hatfull and colleagues are now testing a fourth phage to add to the treatment and looking for ways to apply the technique to other pathogenic bacteria.
“I still have real reservations about whether this kind of approach could be developed into something that could be usable on a large scale,” Marcia Goldberg, an infectious disease specialist at Massachusetts General Hospital, tells STAT. “The amount of science that needs to go into developing a therapeutic against any single strain is huge.”