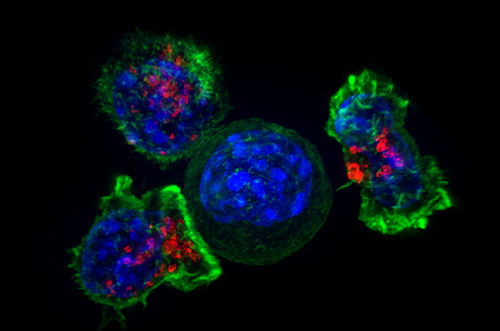
In anticancer campaigns, the immune system has often shown too little fighting spirit. It can be too civilized, too restrained unless it is specially outfitted and guided. Measures that can drive the immune system to exert itself more strenuously, more aggressively, include monoclonal antibodies, cancer vaccines, checkpoint inhibitors, and adaptive cell therapy all the tools and techniques of immuno-oncology.
The proliferation of immuno-oncology tools and techniques was evident at the recent Translating Science into Survival conference. This event, which was held in New York City was organized by the Cancer Research Institute, the Association for Cancer Immunotherapy, the European Academy of Tumor Immunology, and the American Association for Cancer Research. The organizers evidently anticipated that this event, like previous immunotherapy events, would be fairly intimate. Yet it sold out quickly and ultimately strained to accommodate 1,400 attendees.
The event’s popularity was probably at least in partly due to recent immunotherapy successes against blood cancers. For example, adaptive cell therapy approaches have shown promise in small trials, and work along these lines continues apace, as several presentations demonstrated. Moreover, lessons derived from this work may be applied more broadly, even to the treatment of solid tumors.
For example, in a presentation entitled “Engineered T cells for cancer therapy,” the University of Pennsylvania’s Carl June described his team’s progress in using chimeric antigen receptor (CAR)-modified T cells to treat patients with chronic lymphocytic leukemia (CLL). “We previously reported preliminary results on three patients with refractory CLL,” Dr. June noted. “Here we report the mature results for our initial trial using CAR-modified T cells to treat 14 patients with relapsed and refractory CLL.”
The overall response rate in CLL patients was 8/14 (57%), with four complete remissions and four partial remissions. All responding patients developed B cell aplasia and experienced cytokine release syndrome, coincident with T cell proliferation. Minimal residual disease was not detectable in patients who achieved complete remission, which, Dr. June suggested, indicated that “disease eradication may be possible in some patients with advanced CLL.”
Dr. June also summarized a separate investigation that asked whether the CAR cells used against CLL would also be effective against multiple myeloma. At first glance, this may seem odd, since the CAR cells that were effective against CLL target CD19, and CD19 expression is all but absent from myeloma cells. That is, myeloma cells don’t traditionally express CD19 on their surface because they arise from the most mature type of lymphocytes plasma cells.
Dr. June’s team, however, proceeded on the chance that they would be able to incorporate their anti-CD19 CAR T cells into a therapy that would target early precursors of myeloma cells. This therapy, which was administered to a patient with refractory multiple myeloma, involved an infusion of the patient’s own stem cells along with lymphodepleting chemotherapy (melphalan) as well as an infusion (two weeks later) of anti-CD19 CAR T cells.
The patient experienced transplantation-related side effects during the time prior to receiving CTL019, including neutropenia and thrombocytopenia, nausea, fever, and an infection. After receiving the engineered cells, she experienced no fevers or other signs of cytokine release syndrome, a condition that has been observed in other patients undergoing CTL019. At last evaluation, 12 months after treatment, the patient exhibited a complete response with no evidence of progression. According to Dr. June, “This response was achieved despite absence of CD19 expression in 99.95% of this patient’s neoplastic plasma cells.”
While the results presented by Dr. June pertain most directly to blood cancers specifically, the inducement of favorable patient responses to treatment they may also apply more broadly. For example, they demonstrate that a “living drug” may exert its effects indirectly. Also, they emphasize the importance of managing toxicity and ensuring the expansion of modified cells. They also raise the issue of introducing cells that may demonstrate longevity.
More generally, uncertainties surrounding the differential expansion and persistence of distinct cell populations over time can complicate dosing. Similarly, with respect to toxicity, cytokine release and the generation of tumor-shredding products might be considered side effects or, really, evidence that a therapy is working.
Yet engineered cells may also attack both malignant and healthy cells directly. That is, engineered cells may be sensitive to target proteins that stud both cancer cells and also, if only to a lesser degree, normal cells. In CAR T-cell therapies against leukemia and lymphoma, side effects related to direct attacks on normal cells has been manageable. Such side effects, however, may be more severe if adaptive cell therapies are directed against solid tumors.
Leading up to the Translating Science into Survival conference, Dr. June’s group published a study that described an approach for managing target-mediated toxicity. The approach, called affinity tuning, involves generating CAR T cells that are sufficiently insensitive to ignore normal cells, which are relatively target-sparse, and yet sensitive enough to latch onto cancer cells, which are relatively target-rich.
In a paper (“Affinity-Tuned ErbB2 or EGFR Chimeric Antigen Receptor T Cells Exhibit an Increased Therapeutic Index against Tumors in Mice”) that appeared September 1 in Cancer Research, the case was made that “affinity-tuned cells” could exhibit robust antitumor efficacy similar to high-affinity cells, but spare normal cells expressing physiologic target levels: “The use of affinity-tuned scFvs offers a strategy to empower wider use of CAR T cells against validated targets widely overexpressed on solid tumors, including those considered undruggable by this approach.”
At the Translating Science into Survival event, the presentations concerning solid tumors emphasized that adoptive cell therapy could become more effective if obstacles in the tumor microenvironment could be overcome. For example, the University of Pennsylvania’s Ellen Puré, in a presentation entitled, “Tumor stroma: Immunomodulatory functions and a target of immunotherapy,” explained that stroma can be a barrier to T cells, including CAR T cells.
Stromal components such as fibroblasts and the extracellular matrix can play myriad functions in cancer. For example, Puré noted, reactive stroma enriched in growth and angiogenic factors presents chemoattractants that promote the recruitment of bone marrow-derived cells and can modulate inflammatory and immune cell function, all of which can contribute to its tumor-permissive nature relative to normal stroma.
“A significant portion of cancer-associated fibroblasts in virtually all human carcinomas express the cell surface protease fibroblast activation protein (FAP),” Puré continued. “Our studies indicate that FAP+ cells are required for the generation and maintenance of desmoplastic stroma and that depletion of FAP+ cells can inhibit tumor growth through both immune-dependent and immune-independent mechanisms.”
Another take on the tumor microenvironment was presented by Wolf H. Fridman, Cordeliers Research Centre, Paris. In a talk entitled, “Cancer subtypes and their immune microenvironments,” Dr. Fridman described how his group was elaborating on the Immunoscore concept, which goes back at least as far as 2006. Basically, Immunoscore builds on the insight that in many patients, the density of T cells near tumor cells could be a better predictor of survival than traditional staging based on a cancer’s size and spread.
In general, for a patient’s prognosis to be favorable, immune cells need to infiltrate a solid tumor. But recent work also suggests that more immune cells may not always be better. Apparently some immune cells are less helpful than others. Some may even be deleterious, depending on the interactions that occur between a tumor’s microenvironment and the immune system.
“Our team studied the immune infiltrates of pulmonary metastases from colorectal cancer (CRC) and renal cell carcinoma (RCC),” reported Dr. Fridman. “As in primary tumors, a high density of CD8+ T cells correlated with good prognosis for CRC metastases, while it correlated with a bad prognosis for RCC metastases.”
“In addition, in both cancer types, we identified subgroups of poor-prognosis patients with high tumoral lymphocyte infiltration, in the context of high expression of genes related to inflammation, immunosuppression, and angiogenesis,” he continued. “These results suggested that the identity of the tumor cells, rather than the organ where they grow, is critical for shaping the immune contexture of a given tumor.”
A particular cancer, then, may have an ecology of its own, one in which the overall disposition of elements tumor cells, immune cells, extracellular matrix elements, and so on matters, much as the overall disposition of chess pieces matters in a game of chess. Even though it might be advantageous to occupy a particular space on the board, apparently not any chess piece will do. Frustratingly, one’s own pieces may be poorly positioned, so as to get in each other’s way.
Nonetheless, as Dr. Fridman concluded, the integration of molecular and immune tumor phenotypes could guide the selection of immunotherapies “appropriate to specific, potentially responding groups of patients.”