Highlights
•NOTCH signaling is preferentially activated in glioblastoma stem cells
•GSIs have limited activities against glioblastoma stem cells
•FTIs improve response to GSIs in vitro and in vivo
•The combination of FTIs and GSIs makes glioblastoma more sensitive to radiation
Summary
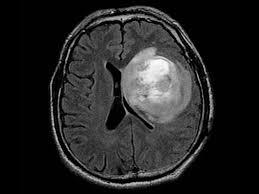
Accumulating evidence suggests that cancer cells with stem cell-like phenotypes drive disease progression and therapeutic resistance in glioblastoma (GBM). NOTCH regulates self-renewal and resistance to chemoradiotherapy in GBM stem cells. However, NOTCH-targeted γ-secretase inhibitors (GSIs) exhibited limited efficacy in GBM patients. We found that farnesyltransferase inhibitors (FTIs) significantly improved sensitivity to GSIs. This combination showed significant antineoplastic and radiosensitizing activities in GBM stem cells, whereas non-stem GBM cells were resistant. These combinatorial effects were mediated, at least partially, through inhibition of AKT and cell-cycle progression. Using subcutaneous and orthotopic GBM models, we showed that the combination of FTIs and GSIs, but not either agent alone, significantly reduced tumor growth. With concurrent radiation, this combination induced a durable response in a subset of orthotopic tumors. These findings collectively suggest that the combination of FTIs and GSIs is a promising therapeutic strategy for GBM through selectively targeting the cancer stem cell subpopulation.
Introduction
Glioblastoma (GBM) is one of the most lethal human malignancies. Despite aggressive surgical resection and chemoradiotherapy, tumor recurrence is nearly universal (Stupp et al., 2005, Wen and Kesari, 2008). It has been increasingly recognized that GBM recurrence is driven by a subset of cells with stem cell-like phenotypes, such as unrestricted self-renewal and the ability to restore cellular heterogeneity (Lathia et al., 2015). These cells are termed as GBM stem cells, but also known as GBM tumor-initiating cells or tumor-propagating cells. The rest of the cellular subpopulation is thought to be the progenies of GBM stem cells and has limited tumorigenic potential. While the identity and plasticity of GBM stem cells remains a subject of debate, these cells appear to be refractory to the current standard of care, including radiation and temozolomide (Bao et al., 2006, Eramo et al., 2006, Pistollato et al., 2010). The abilities of GBM stem cells to evade therapies and to effectively repopulate tumor masses highlight their roles in therapeutic resistance. Hence, these cells are crucial therapeutic targets to achieve prolonged tumor response (Zhu et al., 2014).
There is growing evidence that developmental pathways central to normal stem cell biology, such as those regulated by NOTCH, WNT, and HEDGEHOG, are frequently activated in their malignant counterparts, cancer stem cells (CSCs) (Takebe et al., 2011). Targeting these pathways can be appealing strategies to compromise the CSC subpopulation and improve therapeutic response. The NOTCH signaling pathway has profound indications in development and cancer (Bolos et al., 2007). The canonical NOTCH pathway is mediated through coordinated crosstalk among four NOTCH receptors (NOTCH1–4) and five ligands (Jagged1/2 and DLL1/3/4). Ligand binding induces conformational changes of NOTCH receptors and through a two-step proteolytic cleavage, resulting in nuclear accumulation of the intracellular domains of NOTCH (NICDs) and activation of NOTCH-dependent transcription. The significance of NOTCH activities has been reported in the cancer stem cell subpopulation of GBM and a variety of other cancers (Abel et al., 2014, Fan et al., 2006, Fan et al., 2010, Liau et al., 2017, Saito et al., 2014). Our laboratory has previously demonstrated that NOTCH signaling protects GBM stem cells from radiation (Wang et al., 2010a). Results from other groups also agree that NOTCH signaling may promote resistance to temozolomide and radiation in GBM stem cells (Gilbert et al., 2010, Yahyanejad et al., 2016). NOTCH activity is also implicated in the crosstalk between GBM stem cells and the tumor microenvironment, as expression of NOTCH ligands in endothelial cells within the tumor vasculature supports GBM stem cells (Zhu et al., 2011). In particular, NOTCH activity is required for GBM stem cells to generate endothelial cell-like cells that contribute to tumor angiogenesis (Wang et al., 2010b). Based on these reasons, there has been increasing interest in targeting NOTCH signaling for the treatment of GBM.
The most clinically advanced agents targeting NOTCH are small-molecule inhibitors of γ-secretase (GSIs), which catalyze the second step of releasing NICDs. Based on promising preclinical activities, several GSIs have been examined in clinical trials for cancer patients as monotherapies or in combination with other regimens (Andersson and Lendahl, 2014, Takebe et al., 2015). In a phase I study of MK-0752, a subset of patients with advanced glioma (24%) had prolonged stable disease and there was one case of complete response (Krop et al., 2012). Modest clinical benefits have been shown with other GSIs, such as PF-03084014 and LY900009 (Locatelli et al., 2017, Messersmith et al., 2015, Pant et al., 2016). RO4929097 has been the most widely tested GSI to date. Objective response has been identified in patients with advanced glioma treated with RO4929097 and bevacizumab (Pan et al., 2016). In another clinical study, RO4929097 in combination with the standard chemoradiotherapy reduced the CD133+ fraction of GBM cells and impaired the ability of cancer cells to generate spheres (Xu et al., 2016). However, clinical benefits of GSIs in general are modest at best in patients with advanced glioma or other solid malignancies. Combinations with conventional chemoradiotherapy or other targeted agents to date have offered limited improvement.
Farnesyltransferase inhibitors (FTIs) were originally developed as anti-RAS agents, because farnesylation at the C terminus regulates membrane anchorage of RAS proteins (Appels et al., 2005). While HRAS is strictly dependent on farnesyltransferase, KRAS and NRAS remain functional in the presence of FTIs through geranylgeranylation, an alternative form of prenylation (Sebti and Der, 2003). As such, the exact mechanisms of action of FTIs are still unclear. At least two FTIs, tipifarnib and lonafarnib, have been assessed in patients with GBM, showing modest activities in a small subset of patients (Cloughesy et al., 2006, Haas-Kogan et al., 2011, Lustig et al., 2008, Nghiemphu et al., 2011, Yust-Katz et al., 2013). In the current study, we demonstrated that inhibition of farnesyltransferase significantly improved the efficacy of GSIs in subcutaneous and intracranial GBM models. The combination of FTIs and GSIs made GBM stem cells more sensitive to radiation. Durable response of intracranial tumors in recipient mice was observed following administration of the combination therapy with concurrent radiation.
Results
GSIs as Monotherapy Have Limited Activities in GBM Stem Cells
We have previously demonstrated that targeting NOTCH in GBM stem cells with GSIs, such as DAPT and L685,458, induced only modest growth inhibition (Wang et al., 2010a). To improve NOTCH-based therapy for GBM, we investigated the therapeutic potential of a highly potent and brain-penetrating GSI, RO4929097. GBM stem cells were isolated from patient-derived xenograft (PDX) models and enriched by magnetic sorting for the CD133 cell surface marker. These CD133+ cells expressed higher levels of stem cell markers, such as MYC, and lower levels of differentiation markers, such as GFAP, compared with matched CD133− cells (Figure S1A). Cleaved NOTCH1 was higher in CD133+ cells, suggesting that NOTCH was preferentially activated in this subpopulation (Figure 1A). Consistently, CD133+ cells also expressed higher levels of canonical NOTCH target genes, HES1 and HES2 (Figure S1B). In addition, NOTCH1 and NOTCH2 mRNA levels were higher in CD133+ cells (Figure S1B). Despite preferential activation of NOTCH signaling in CD133+ cells, RO4929097 had only modest impact on the viability of these cells (Figures 1B and S1C). In contrast, matched CD133− cells were essentially unresponsive to RO4929097 (Figures 1B and S1C). Although the impact on proliferation was limited, RO4929097 significantly undermined tumor sphere formation (Figure 1C), suggesting specific functions of NOTCH in the regulation of self-renewal in GBM stem cells. Measured by limiting dilution assays, RO4929097 significantly reduced the frequency of self-renewing cells in the CD133+ subpopulation (Figures 1D–1F). However, these results suggest that blockade of NOTCH signaling alone may not be sufficient to effectively kill GBM stem cells.
FTIs Synergistically Augment Cytotoxicity of GSIs In Vitro
To identify agents that might potentiate the toxicity of GSIs against GBM stem cells, we tested a set of targeted agents that had been previously evaluated in GBM patients (Wang et al., 2015). Our results showed that RO4929097 significantly reduced the LC50 values, defined as the concentrations causing loss of 50% cell viability, for a farnesyltransferase inhibitor, tipifarnib, and two other compounds targeting the EGFR family receptors (Table S1). Tipifarnib was selected for further study as it induced significant cell death in the presence of RO4929097. Our data showed that both tipifarnib and RO4929097 alone at physiologically relevant concentrations significantly reduced CD133+ cells growth and induced modest apoptotic cell death (Figures 2A–2C ), whereas the combination showed stronger anti-proliferative effects and cytotoxicity compared with single agents (Figures 2A–2C and S2A). In contrast, CD133− cells were largely resistant to tipifarnib and RO4929097, either alone or in combination (Figures 2C, 2D, S2A, and S2B).
We next asked whether the interaction between tipifarnib and RO4929097 was synergistic. To calculate the drug synergy, T4302 CD133+ cells were treated with tipifarnib, RO4929097, or the combination of these two compounds mixed at an equal molar ratio following a 3-fold serial dilution. The LC50 value for tipifarnib in T4302 CD133+ cells was 32 nM when combined with RO4929097 compared with 194 nM as a monotherapy (Figure 3A). The loss of cell viability induced by RO4929097 alone was not greater than 50%. On the basis of cell viability data, drug synergy was calculated across a wide range of concentrations using the Chou-Talalay statistical method (Chou, 2010). The combination index (CI) values were markedly lower than 1 at drug concentrations above 1 nM, indicating strong drug synergy (Figure 3B). In contrast, T4302 CD133− cells were refractory to tipifarnib and RO4929097, either alone or combined (Figure 3C). Similar synergistic response was shown in T4105 CD133+ cells as well as spheroid cultures derived from low-passage GBM PDX models, but not T4105 CD133− cells (Figures 3D, 3E, S3A, and S3B). In line with these findings, additional FTIs and GSIs, such as L744,832 and DAPT, also exhibited synergistic interactions (Figure S3C). Conversely, the synergism between tipifarnib and RO4929097 was absent in normal human neural progenitor (NHNP) cells (Figure S3D). Not all GBM stem cells were sensitive to this combination therapy. Examination of additional GBM stem cell lines generated in vitro showed that only one proneural subtype line was sensitive (Wang et al., 2017), while the other three lines were not (Figures S3E–S3H). Limiting dilution assays showed that the combination therapy had a profound impact on the self-renewal capacity of GBM stem cells. While approximately 1 out of 2 T4302 CD133+ cells had self-renewal capacity (Figures 3F and 3G), exposure to 100 nM tipifarnib or RO4929097 reduced the frequency of self-renewing cells to 1 out of 8.57 or 3.84, respectively, while the combination reduced the ratio of self-renewing cells to 1 out of 31.02. Similar observations were made in T4105 CD133+ cells (Figures 3F and 3H). Taken together, our results suggest that inhibition of farnesyltransferase synergistically and selectively enhances the efficacy of GSIs in a subset of GBM stem cells.
The Combination of Tipifarnib and RO4929097 Suppresses Key Signal Transduction Pathways and Cell-Cycle Regulators
NOTCH signaling is known to crosstalk with a wide range of signal transduction pathways that result in tumor-promoting or tumor-suppressive activities in a context-dependent manner (Ranganathan et al., 2011). Inhibition of farnesyltransferase also affects many pathways through modulation of farnesylation of crucial signaling molecules, including the RAS family of GTPases (Sebti and Der, 2003). To interrogate the mechanisms mediating the cytotoxicity of the combination of tipifarnib and RO4929097, we first tested the impact on the PI3K/AKT pathway and the MAPK pathway in GBM stem cells. Although the patterns of changes in these two pathways were not identical in GBM stem cells derived from different PDX models, the combination was more effective to reduce the phosphorylation levels of AKT and ERK than either agent alone (Figure 4A). Overexpression of a constitutively active myristoylation signal-linked AKT1 (Myr-AKT1) increased the LC50 of the combination therapy from 101 nM to 330 nM (Figure 4B). Of note, tipifarnib induced a modest upregulation of cleaved NOTCH1, suggesting that NOTCH activation may be implicated in resistance to FTIs. Consistent with this hypothesis, ectopic expression of a constitutively active intracellular domain of NOTCH1 (NICD1) reduced tipifarnib-induced caspase activation (Figure 4C).
To interpret the global impact of this combination therapy, we employed microarray to assess changes in gene expression profiles induced by the combination of tipifarnib and RO4929097. Gene set enrichment analysis (GSEA) showed that several gene signatures implicated in cell-cycle regulation were consistently downregulated by the combination of tipifarnib and RO4929097 (Figure S4A). The combination also suppressed gene sets dependent on the E2F family transcription factors (Figure S4B), which include many genes implicated in cell-cycle regulation. Quantitative real-time PCR (qRT-PCR) was used to validate the changes in selected cell-cycle regulatory genes, including Aurora kinase A/B (AURKA and AURKB), CDC25C, and BUB1. These genes were significantly downregulated by tipifarnib in T4105 and T4302 CD133+ cells (Figures 4D and S5A). However, RO4929097 did not significantly affect expression of these targets. Consistently, tipifarnib reduced the fraction of cells in S phase and increased the subpopulation of cells in G1 phase, while RO4929097 had limited impact on cell-cycle progression (Figures 4E and S5B). To determine the role of cell-cycle progression in mediating the drug synergy, we asked if RO4929097 affected the responsiveness of CD133+ cells to compounds that impaired cell-cycle progression. Our data showed that RO4929097 made both T4105 and T4302+ CD133+ cells more sensitive to the CDK4/6 inhibitor, palbociclib, or the AURKB inhibitor, barasertib (Figures 4F, 4G, S5C, and S5D). These results suggest that the ability of FTIs to compromise cell-cycle progression is critically implicated in the synergistic interaction with GSIs. A recent study suggested that NOTCH signaling might antagonize neuronal differentiation in a subset of GBM stem cells through suppressing expression of ASCL1, a transcription factor promoting neurogenesis (Park et al., 2017). Our data showed that RO4929097, either alone or combined with tipifarnib, did not induce expression of ASCL1 or neuronal markers, such as TUBB3 and MAP2 (Figure S5E), suggesting that an ASCL1-dependent transcription program may not be the target of this combination therapy in our model systems.
Tipifarnib Augments the In Vivo Activities of RO4929097
The in vivo activities of tipifarnib, RO4929097, and the combination were first assessed in subcutaneous GBM tumors. Either tipifarnib or RO4929097 alone had limited impact on tumor growth. Conversely, the combination significantly reduced the growth of T4105 xenograft tumors (Figure 5A). Two weeks following treatment, the median size of T4105 tumors in the combination group was approximately 24% of the vehicle group (Figure 5A). Because both tipifarnib and RO4929097 penetrate the blood-brain barrier (Nghiemphu et al., 2011, Xu et al., 2016), we further evaluated their combinatorial effects in orthotopic GBM models. At the doses used in our experiments, tipifarnib induced significant accumulation of PRELAMIN A (Figure S6A), a marker of farnesyltransferase inhibition. RO4929097 reduced the levels of cleaved NOTCH1 (Figure S6B), indicating blockade of NOTCH signaling. The median survival of mice carrying intracranial T4302 tumors was marginally increased by either tipifarnib or RO4929097 (Figure 5B). In contrast, the combination of these two compounds extended the median survival by 25% compared with the group treated with vehicle (40 versus 32 days, p = 0.018 by the log rank test) (Figure 5B). No significant weight loss was associated with administration of tipifarnib, RO4929097 or the combination (Figure S6C). However, intracranial tumor burdens induced weight loss at the late stage of the experiments. These findings indicate that combining inhibitors of farnesyltransferase and γ-secretase may produce more potent therapeutic activities in GBM than monotherapies.
Concurrent Inhibition of Farnesyltransferase and γ-Secretase Improves Radiosensitivity
We have previously reported that inhibition of NOTCH using GSIs or RNAi improved radiosensitivity of GBM stem cells (Wang et al., 2010a). Several other preclinical studies also showed that GSIs made GBM more sensitive to standard chemotherapy and radiation (Dantas-Barbosa et al., 2015, Gilbert et al., 2010, Yahyanejad et al., 2016). In addition, the fraction of tumor cells positively stained for NOTCH1 was higher in recurrent GBM samples compared with matched primary tumors (Saito et al., 2015). Radiosensitizing activities have also been reported for FTIs in preclinical models, including tipifarnib (Appels et al., 2005). Therefore, we asked whether targeting both farnesyltransferase and γ-secretase would further improve sensitivity to radiation in GBM stem cells. While both tipifarnib and RO4929097 significantly decreased the viability of irradiated CD133+ cells, the combination of two compounds resulted in nearly complete eradiation of CD133+ cells with concurrent radiation (Figure 6A and S7A). A 3-Gy ionizing radiation reduced the LC50 values of the combination from 90.6 nM to 33.2 nM in T4105 CD133+ cells and from 33.1 nM to 11.2 nM in T4302 CD133+ cells (Figures 6B and S7B–S7D). The CI values in irradiated T4302 CD133+ cells were also substantially lower than those in cells that were not irradiated (Figure 6C).
The in vivo radiosensitizing effects of the combination therapy were examined using orthotopic GBM models. Mice bearing intracranial T4302 tumors were irradiated 4 hr after the first dose of tipifarnib, RO4929097, or the combination. This treatment was repeated once on the next day. Subsequently, mice were treated daily with tipifarnib and/or RO4929097 until those in the control group exhibited significant neurological signs. Tipifarnib did not extend the survival of tumor-bearing mice following radiation, while RO4929097 increased the median survival by approximately 10% (45 days versus 41 days, p = 0.012) (Figure 6D). Interestingly, one mouse in the RO4929097 arm remained healthy at the end of the experiment and showed no signs of tumor burden in the brain. The combination of tipifarnib and RO4929097 extended the median survival by approximately 22% (50 versus 41 days, p = 0.004). In this group, one mouse lived for 97 days after tumor implantation prior to developing severe neurological signs. Another mouse was also disease free at the end of the experimental endpoint (120 days). Weight loss at the end of treatment was likely associated with disease progression (Figure S6C). Taken together, these results suggest that the combination of FTIs and GSIs may improve the response to radiotherapy in GBM and induce durable tumor response, potentially through targeting the cancer stem cell subpopulation.
Discussions
GSIs have been assessed in a wide variety of cancers either as a monotherapy or in combination with conventional chemoradiotherapy. Monoclonal antibodies targeting NOTCH receptors or ligands are also in development (Takebe et al., 2015). However, the overall clinical benefits of NOTCH-targeted therapies appear to be modest and transient. Combination approaches hold the promise to improve the outcomes of NOTCH-targeted agents. For example, targeting both EGFR and NOTCH generated synergistic toxicity and reduced the fraction of CSCs in breast cancer and lung cancer models (Dong et al., 2010, Hu et al., 2017). Synergism between GSIs and CDK inhibitors has been reported in acute lymphoblastic leukemia (Rao et al., 2009). NOTCH activity played a critical role to protect GBM stem cells following exposure to PDGFR inhibitors or EGFR inhibitors (Liau et al., 2017). These findings also suggest that mechanisms mediating resistance to NOTCH-targeted therapies may be context dependent. In the current study, we identified a combination therapy of GSIs and FTIs that selectively and synergistically targeted GBM stem cells in vitro. This combination was more effective in vitro and in vivo compared with either agent alone, and when administrated together with radiation, could result in prolonged tumor control in mice carrying intracranial GBM tumors.
NOTCH activation has been increasingly described in the CSC subpopulation of GBM and other cancers (Bolos et al., 2009, Lathia et al., 2015). We demonstrated that CD133+ GBM cells expressed higher levels of NOTCH receptors and canonical NOTCH target genes compared with matched CD133− cells. In line with differential NOTCH activation, CD133+ GBM cells responded to RO4929097 at nanomolar concentrations, while CD133− cells were highly resistant. However, RO4929097 alone had limited activities in GBM stem cell cultures or xenograft models. The cytotoxicity of RO4929097 in GBM stem cells was significantly increased when combined with FTIs. Conversely, RO4929097 did not have a significant impact on differentiated GBM cells either alone or in combination with tipifarnib. Both RO4929097 and tipifarnib have been examined in clinical trials of various hematopoietic and solid cancers. RO4929097 has modest activities in a small subset of patients (De Jesus-Acosta et al., 2014, LoConte et al., 2015, Pan et al., 2016, Sahebjam et al., 2013, Tolcher et al., 2012). Although development of this compound was discontinued due to CYP3A4 auto-induction, other NOTCH-targeted agents are under development (De Jesus-Acosta et al., 2014, Tolcher et al., 2012). The clinical efficacy of tipifarnib was also limited in GBM and other cancer types, despite promising preclinical activities (Ducassou et al., 2013, Moyal et al., 2007, Nghiemphu et al., 2011). Our data agreed that neither RO4929097 nor tipifarnib alone had significant activities in subcutaneous and orthotopic GBM models. In contrast, the combination of these two compounds effectively reduced tumor growth and improved survival of mice carrying intracranial tumors. Although the combination therapy is expected to affect the diverse substrates of farnesyltransferase and γ-secretase, mice treated with the combination did not show significant weight loss, suggesting that these two classes of compounds may be safely combined.
GBM stem cells were highly sensitive to radiation in the presence of both FTIs and GSIs. Results from our laboratory and several other groups have demonstrated that blockade of NOTCH signaling rendered GBM stem cells more sensitive to radiation or temozolomide (Dantas-Barbosa et al., 2015, Gilbert et al., 2010, Shen et al., 2015, Yahyanejad et al., 2016). Similar findings have been reported in several additional cancer types (Aleksic and Feller, 2008, Lagadec et al., 2013, Mizugaki et al., 2012). Based on these preclinical studies, RO4929097 has been evaluated in combination with the standard chemoradiotherapy in patients with newly diagnosed advanced glioma (Xu et al., 2016). With concurrent temozolomide and radiation, RO4929097 reduced NOTCH activity in tumors and decreased the fraction of CD133+ cells (Xu et al., 2016). Tipifarnib has also been tested concurrently with chemoradiotherapy in GBM patients, but the benefits were limited (Nghiemphu et al., 2011). Our data suggest that either RO4929097 or tipifarnib alone did not significantly improve the response to radiation in the orthotopic GBM model, although one outliner could have been cured with RO4929097 plus radiation. In contrast, the drug combination with concurrent radiation significantly extended the median survival of experimental animals with two cases of durable response. The response of intracranial tumors is consistent with the sensitivity of cultured GBM stem cells to the combination therapy. In contrast, non-stem GBM cells in culture were highly resistant, which appeared to be irrelevant to the outcomes. However, response to the combination therapy with concurrent radiation drastically varied among the experimental animals. One possibility is that two doses of radiation plus the drug combination only had a slight chance to successfully eradicate GBM stem cells, whereas a very small number of surviving CSCs could lead to rapid repopulation of the tumors. As such, further optimization of this combination therapy, such as increasing the number of radiation doses, is necessary to fully understand the therapeutic potential of the combination of GSIs and FTIs. Taken together, our results suggest that the therapeutic response of cultured GBM stem cells may be recapitulated in preclinical models of GBM. Further preclinical optimization and clinical development are needed to determine whether these encouraging findings can be translated into significant clinical benefits.
Although the role of NOTCH in CSCs has been reported by many laboratories, GSIs may affect a variety of substrates of γ-secretase in addition to NOTCH (Haapasalo and Kovacs, 2011). Our data suggest that inhibition of both farnesyltransferase and γ-secretase results in more effective suppression of AKT and MAPK signaling than either agent alone. FTIs were initially developed to target RAS proteins through inhibition of their farnesylation and membrane interaction (Appels et al., 2005). However, alternative prenylation of KRAS renders KRAS-mutant cancers largely insensitive to FTIs. Our results suggest that FTIs may modulate upstream regulators of AKT and MAPK in GBM stem cells when combined with GSIs. We also showed that FTIs reduced expression of several cell-cycle regulators and impaired cell-cycle progression. FTIs have been shown to increase radiosensitivity through targeting the G2/M checkpoint mechanisms (Song et al., 2000). Another farnesyltransferase substrate, small GTPase RhoB, is also known to regulate tumor response to radiation through mitosis (Milia et al., 2005). Our data showed that multiple kinase inhibitors targeting cell-cycle regulators partially recapitulated the ability of FTIs to augment response to GSIs. Hence, regulation of cell-cycle progression appears to be another important mechanism implicated in the interaction between FTIs and GSIs.
To summarize, our study identified a combination therapy of FTIs and GSIs that selectively target the cancer stem cell subpopulation in GBM. This combination therapy with concurrent radiation induced a durable response in orthotopic GBM models. The compounds tested in our study included two experimental agents that have shown modest efficacy in patients with advanced glioma. Although clinical development of RO4929097 and tipifarnib has been discontinued, our results suggest a potential revisit of NOTCH-targeted therapy with the objective to improve the response of GBM to the standard chemoradiotherapy.