arly in the pandemic, some believed that the arrival of summer would make COVID-19 cases drop, much like the flu. In March 2020, Brazil’s president Jair Bolsonaro implied that his country should not expect a COVID-19 crisis like that in Italy at the time, given the “totally different” climates of the two places. “Maybe this goes away with heat and light,” said then–US President Donald Trump the following month.
But the increased number of cases in the US and other countries in the Northern Hemisphere in the summer of 2020 contradicted these predictions. Moreover, the tropics were not spared from high death tolls, despite their lack of wintry weather. Brazil and India emerged, for instance, as two of the leading pandemic hotspots.
These events illustrate that climate has not governed whether COVID-19 emerges or vanishes in a given place or time. But nearly two years after the first reported cases, the available data are allowing researchers to better explore the role of meteorological factors in case numbers, and their results point to low temperature, low humidity, and limited sunlight as conditions that foster the spread of SARS-CoV-2. Currently, factors such as human behavior outweigh the influence of weather, but experts say it’s likely that COVID-19 will eventually be a seasonal disease.
COVID-19’s seasonal signatures
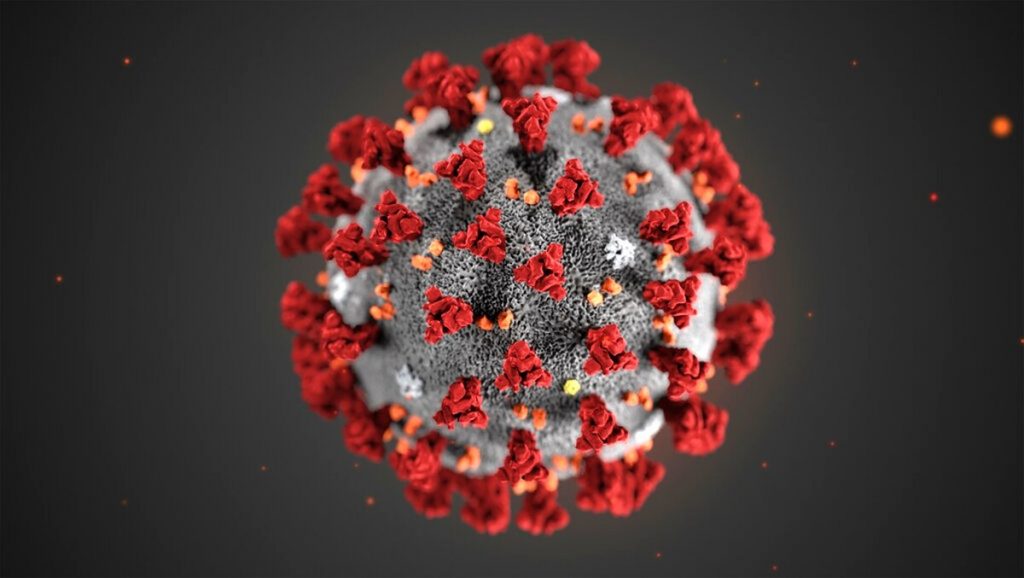
“We cannot rely on climate to make SARS-CoV-2 to disappear,” says Sen Pei, an epidemiologist at Columbia University. But while that’s now clear, early on there were reasons to suspect that SARS-CoV-2 was sensitive to temperature and other climatic factors. These included the fact that respiratory infections tend to be seasonal, and that the new virus’s structure seemed likely to be sensitive to temperature, humidity, and sunlight.
In 2020, various research groups began trying to ferret out whether there was a role for climate in COVID-19, but given the limited data available then, they did not reach a consensus. For instance, positive, negative, and nonsignificant associations were observed between temperature and viral transmission by different teams. More recent studies have been more consistent in identifying negative correlations between temperature and transmission, although the degree of its influence is still a subject of debate.
Pei and his colleagues, for instance, estimated this June that the combined effects of temperature, humidity, and ultraviolet radiation explain 17.5 percent of SARS-CoV-2 transmission in 2,669 US counties from March to December 2020. Two global studies by different groups, published in October 2021, also concluded that weather matters, although one identified temperature and humidity as strong drivers of transmission during specific periods of time—as in other climate-sensitive diseases—while the second found only a modest role for these factors and emphasized that government interventions in the early stage of the pandemic appeared to be much more determinant.
One of the multinational analyses was led by Barcelona Institute for Global Health (ISGlobal) climate and health scientist Xavier Rodó, who has previously studied the relationship between climatic factors and diseases such as cholera, malaria, and seasonal flu. His team has identified that in such seasonal diseases, weather and transmission are coupled transiently—that is, factors like temperature and humidity influence the incidence of cases for specific periods of time. These couplings, however, may last only a few days, or weeks at most, followed by periods where little or no association is observed, explains Rodó.
Climatic process “tend to act in the form of thresholds,” he says. For instance, above or below a specific temperature or humidity level, intense short-term transient associations between meteorological variables and case numbers are more likely to be detected.
Using data from 162 countries collected from March to October 2020, Rodó and colleagues looked for this pattern in COVID-19, searching for transient couplings in time windows of different lengths (from 14 to 75 days) and across different space scales (country, region, and city). They found consistent negative associations between temperature and humidity and COVID-19 cases, especially in the first two pandemic waves. Strong correlations were also more common at temperatures between 12 and 18°C. These temporal associations sometimes accounted for more than 80 percent of the total variability in cases in three regions they zoomed in: Lombardy in Italy, Thüringen in Germany, and Catalonia in Spain.
The influence of these meteorological factors acts “on top of other processes,” such as the behavior of people, given the nature of the disease and how it is transmitted, he adds. But Rodó foresees that “in certain latitudes, essentially in the temperate climates,” weather may become one of the main factors driving the disease if community transmission levels are low.
“The strength of this study is that they applied this method to many different countries . . . with various control measures,” says Pei, and “if they observe consistent patterns in the seasonality, that is an indication that maybe the virus has some seasonality there.”
Weather matters, to a point
Temperature and humidity affect SARS-CoV-2 transmission, but government interventions’ impact was six times greater early in the pandemic, concluded the other international study published in October, which focused on the first wave of COVID-19 in 409 cities across 26 countries (using data collected from February to April 2020).
Francesco Sera, a statistician and epidemiologist who worked on the study while at the London School of Hygiene and Tropical Medicine, explains that the team characterized the epidemic growth for each city in the first 20 days after the first locally-transmitted cases were detected there. The researchers analyzed that growth along with contemporaneous environmental data, while controlling for socioeconomic variables such as population density and gross domestic product, and pollution levels. Importantly, he adds, they also considered government measures to combat the virus, as drawn from the Oxford COVID-19 Government Tracker.
The team’s analysis found that temperature and humidity accounted for 2.4 and 2 percent of the variation in transmission rates, respectively, based on the effective reproductive number. In contrast, government policy responses such as school closures, restrictions on gatherings, and testing programs explained 13.8 percent of that variability.
“Overall the methods [used by Sera and colleagues] are very robust,” says Maggie Sugg, an environmental health scientist at the Appalachian State University who was not involved in the study. “Climate is just one small part of the puzzle,” she adds, but nonetheless it is important to understand its role, in order to tackle COVID-19 “from every angle.”
Although they ask a similar question, the two multinational studies use different methodologies and focus on different locations and different stages of the pandemic. Thus, it isn’t possible to closely compare their results, but according to Pei, “the consistent readout” for both papers and his own work is that “the transmissibility of SARS-CoV-2 is certainly modulated by climate factors like temperature, humidity,” but that these are not currently the dominant factors driving it.
“Both of these studies are some of the best in the field right now in terms of trying to pinpoint an effect,” says Princeton University epidemiologist Rachel Baker, who did not participate in either of them or Pei’s earlier study. “They are using some of the best approaches out there” to understand the impact of weather in COVID-19, yet it is a “tricky signal to detect right now.” She explains that a lot of data is needed to detect such a signal—for instance, to compare warmer versus colder years—so it may yet be too early to reach an absolute conclusion on the seasonality of COVID-19.
As SARS-CoV-2 is an emergent pathogen, it has “colonized everything” on its way, says Rodó, and thus we have it in winter and summer, in colder and warmer locations. During this early stage, the high number of susceptible people has been a more fundamental driver of the pandemic than weather, according to a modeling study Baker and her colleagues published last summer. It might be, she says, that “only after population immunity increases over time” will we see a more evident “climate signature and more seasonal patterns of outbreaks.”
A preference for cold, dry, and not too sunny
In addition to epidemiological studies identifying the role of meteorological factors in SARS-CoV-2 transmission, the virus’s behavior inside the lab points to a preference for winterlike conditions. In lab experiments, higher intensity of simulated sunlight, higher temperature, and higher humidity result in a faster decay of the virus in aerosols.
“We know that at low relative humidity, [aerosols] dry out,” explains University of Nebraska Medical Center aerosol scientist Shanna Ratnesar-Shumate, and this seems to contribute to the infectivity of the virus. Changes in temperature and humidity within the aerosols may be either friendly or toxic to the virus, but what exactly happens within that microenvironment under those changes is not yet entirely understood.
But the climate-dependent survival of SARS-CoV-2 in the aerosols may not be the only explanation for its success in cold and dry environments in real life. Independently of what happens to the virus within these particles, other factors may contribute to its higher infectivity at certain temperature and humidity levels. For instance, aerosols shrink in dry environments, which allows them to float around more easily, increasing the chances that the viral particles inside will infect someone. Additionally, small aerosols “can bypass the barriers in the respiratory system, so they can reach to the deeper parts of the lungs,” says Rodó.
Regardless the specific chemical, physical, and physiological explanation for the virus’s weather preference, Ratnesar-Shumate says that judging by the results of laboratory studies on the seasonal flu and those on SARS-CoV-2, “there’s really nothing that lends to one being different from the other in terms of [their] seasonality.” Furthermore, we know other, cold-causing coronaviruses are also seasonal. Thus, she says she thinks that COVID-19 will eventually converge on seasonality.
A disease of winter?
While Rodó and his colleagues conclude that COVID-19 is a “seasonal low-temperature infection,” Sera, who is now at the at the University of Florence, argues that “we need more time”—many more years of observation, before that can be known for certain.
Rodó concedes that COVID-19 “has not yet organized as a normal seasonal disease.” But seasonal outbreaks nevertheless are occurring, he adds, as winter conditions in some places facilitate airborne transmission, which he says can affect infection rates “even though you can have the process being dominated” by other factors.
Whether this year will see a winter wave in the Northern Hemisphere will depend on several factors, Pei says. These include the percentage of the population with immunity (due to vaccines or previous infection), possible new variants, and human behavior. If a decline in case numbers leads people to relax their social distancing and other protective measures, this will create “more opportunity of transmission in the winter,” he says.
As Sera and his colleagues conclude in their paper, there are no climate conditions that could impede SARS-CoV-2 transmission if preventive measures are not taken. But knowing that the virus is likely “more transmissible in winter,” we may want “to take better precautions” this time of the year, advises Pei.