Scientists from Fred Hutchinson Cancer Research reported data from an early-phase study of patients with advanced non-Hodgkin’s lymphoma (NHL) who received JCAR014, a chimeric antigen receptor (CAR) T-cell treatment, and chemotherapy.
Their paper “Immunotherapy of Non-Hodgkin’s Lymphoma with a Defined Ratio of CD8+and CD4+ CD19-Specific Chimeric Antigen Receptor–Modified T Cells,” published in Science Translational Medicine, described the results of the first 32 patients in a dose-finding trial of JCAR014 following a round of chemotherapy, called lymphodepletion, designed to create a more favorable environment for the CAR T cells to grow in the patient’s body. Key findings of the study demonstrated the importance of the choice of lymphodepletion regimen and the effects of different doses of CAR T cells.
A total of 50% of the 18 patients who were evaluable for efficacy after receiving CAR T cells and chemotherapy agents fludarabine and cyclophosphamide (Cy/Flu) had a complete response, which compares favorably to the 8% complete response rate in patients who received JCAR014 plus cyclophosphamide-based chemotherapy without fludarabine. As previously reported, dose-limiting toxicities were observed in some patients in this dose-finding study who received the highest CAR T-cell dose. The study continues with the intermediate CAR T-cell dose.
In patients that received Cy/Flu lymphodepletion and the intermediate dose of JCAR014, the data showed a promising early efficacy and side effect profile. Specifically, the overall response rate was 82% (9/11), the complete response rate was 64% (7/11), the severe cytokine release syndrome was 9% (1/11), and severe neurotoxicity was 18% (2/11)
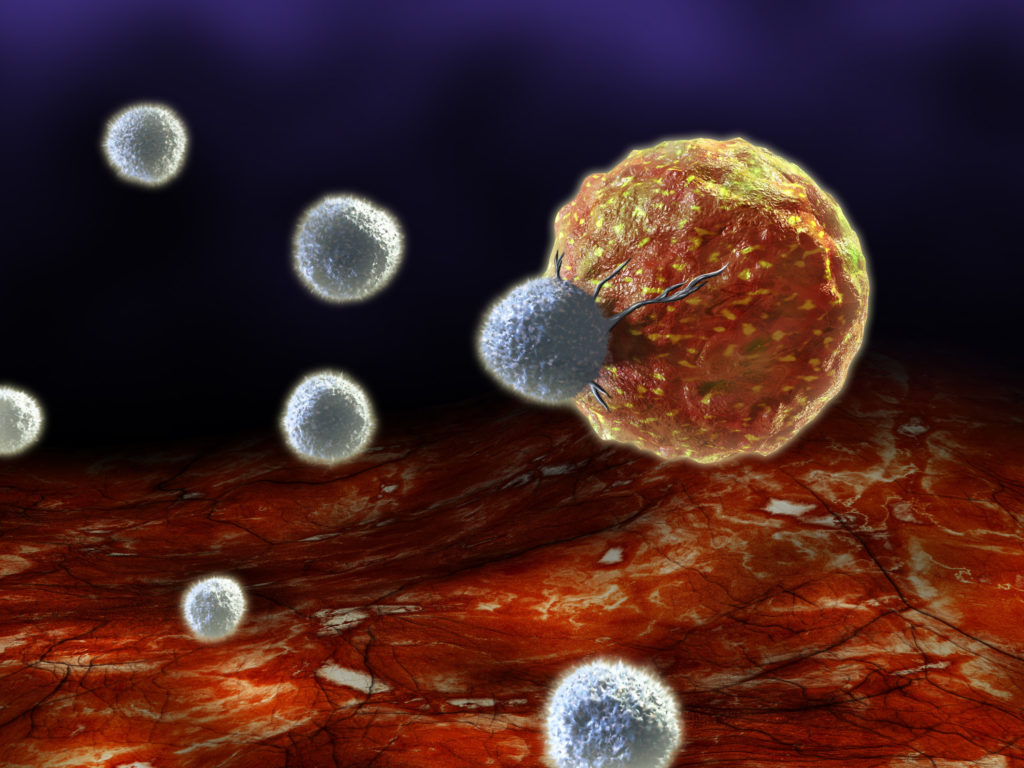
JCAR014’s hallmark is its use of a one-to-one ratio of helper (CD4+) and killer (CD8+) CAR T cells, which join forces to kill tumor cells that produce CD19, a molecule found on the surface of many blood cancer cells, including lymphoma and leukemia. By controlling the mixture of T cells that patients receive, the researchers can see relationships between cell doses and patient outcomes that were previously elusive. The data also suggest that with a defined one-to-one composition of cells, efficacy of treatment is increased, while toxic side effects are minimized.
“With the defined composition treatment, we are able to get more reproducible data about the effects of the cells—both the beneficial impact against the cancer and any side effects to the patient,” said Fred Hutch clinical researcher Dr. Stan Riddell, one of the senior authors of the paper, along with Dr. David Maloney. “We are then able to adjust the dose to improve what we call the therapeutic index—impact against the tumor, with lower toxicity to the patient.”
“This study shows that at the right dose of CAR T cells and lymphodepletion, we can achieve very good response rates for NHL patients who have no other treatment options,” said Cameron Turtle, Ph.D., an immunotherapy researcher at Fred Hutch and one of the study leaders.
Juno said results from the study will be key to its development of another CAR-T candidate, JCAR017, which is also focused on treating CD19 positive blood cancers.
In July, Juno acknowledged in a regulatory filing that four patients had died in trials related to its CAR T-cell candidates. One death occurred during the JCAR014 trial—a young adult patient with relapsed or refractory acute lymphoblastic leukemia (ALL) who received the combination of cyclophosphamide and fludarabine preconditioning, and a higher JCAR014 cell dose than was later used in that trial. Juno said it disclosed that death in data presented at the American Society of Hematology meeting in December 2015, and included in Juno’s Form 10-K Annual Report for 2015.
The other three took place during the Phase II ROCKET trial of its ALL candidate JCAR015. The JCAR015 deaths—all instances of cerebral edema in patients under age 25—led the FDA to briefly impose a partial clinical hold on the ROCKET trial, a hold that was lifted less than a week later after Juno agreed to modify the protocol to cyclophosphamide alone.