Abstract
Sterile inflammation after injury is important for tissue restoration. In injured human and mouse tissues, macrophages were recently found to accumulate perivascularly. This study investigates if macrophages adopt a mural cell phenotype important for restoration after ischemic injury. Single-cell RNA sequencing of fate-mapped macrophages from ischemic mouse muscles demonstrates a macrophage-toward-mural cell switch of a subpopulation of macrophages with downregulated myeloid cell genes and upregulated mural cell genes, including PDGFRβ. This observation was further strengthened when including unspliced transcripts in the analysis. The macrophage switch was proven functionally relevant, as induction of macrophage-specific PDGFRβ deficiency prevented their perivascular macrophage phenotype, impaired vessel maturation and increased vessel leakiness, which ultimately reduced limb function. In conclusion, macrophages in adult ischemic tissue were demonstrated to undergo a cellular program to morphologically, transcriptomically and functionally resemble mural cells while weakening their macrophage identity. The macrophage-to-mural cell-like phenotypic switch is crucial for restoring tissue function and warrants further exploration as a potential target for immunotherapies to enhance healing.
Main
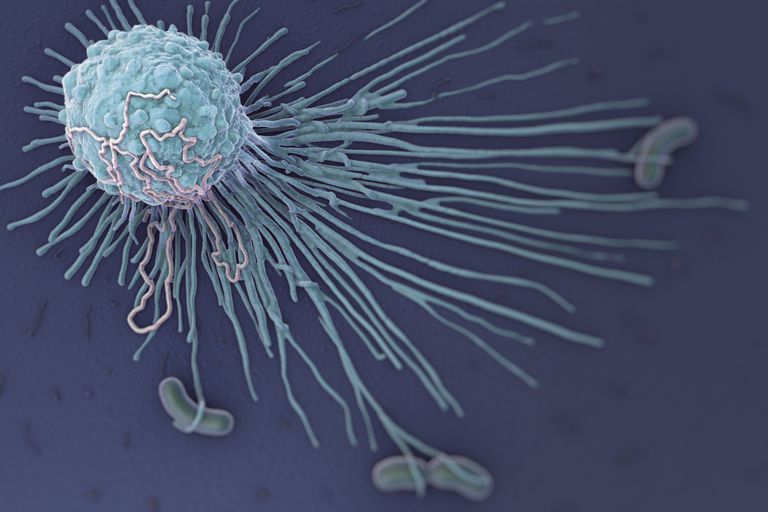
The unique properties of macrophages include their ability to traffic to and accumulate at distinct locations upon infection or tissue injury to exert their effector functions. In injured, ischemic tissues, these effector functions encompass clearing the site from dead and damaged cells1 as well as contributing to the formation of new vessels by paracrine release of growth factors and enzymes2,3,4,5. The first cells to arrive to the injured tissues are neutrophils, monocytes and macrophages, where the short-lived neutrophils are most numerous during the first couple of days after insult, whereas macrophages remain at the site and polarize into different subsets with distinct functions in response to environmental instructions6,7. Different macrophage subsets are, therefore, thought to contribute to restoration of tissue perfusion by separate means, for example by clearing the site of injured cells, as well as by producing distinct growth factors to promote angiogenesis and vessel stabilization8,9. To date, the wide range of known macrophage functions are attributed to their ability to switch into subsets within their lineage. Whether macrophages of adult tissues can adopt functions of other cells by initiating transdifferentiation has not been demonstrated.
Manifestations of cardiovascular diseases are caused by impaired tissue perfusion and subsequent injury and loss of tissue function. Rapid re-establishment of functional blood flow is critical after an ischemic event to limit the extent and severity of tissue damage as well as to allow for healing and regaining function. Formation of new blood vessels from existing ones, known as angiogenesis, is promptly initiated after ischemia onset and occurs in parallel with an inflammatory response provoked by the damaged tissue9. Angiogenesis is a highly complex process that involves degradation of the capillary basement membrane, endothelial cell proliferation and directed migration, followed by tube formation and vessel fusion10. Macrophages contribute to angiogenesis by producing vascular endothelial growth factor A (VEGF-A) and by degrading extracellular matrix (ECM)9,11. To regain functional perfusion, these vessels then need to stabilize and mature, which requires recruitment of perivascular mural cells (pericytes and smooth muscle cells) in a platelet-derived growth factor BB (PDGF-BB)-dependent (secreted by endothelial cells) and a platelet-derived growth factor receptor beta (PDGFRβ)-dependent (on the surface of mural cells) manner12,13. In a model of renal injury, macrophages were shown to support the recruitment of pericytes by secreting PDGF-BB14. During homeostasis, pericytes and vascular smooth muscle cells regulate vessel permeability and blood flow, respectively, and genetic models of mural cell loss result in hemorrhagic and dilated vessels, leading to lethality before birth13,15. So far, therapeutic means to improve the formation of functional blood vessels by upregulating growth factors or chemokines at the site of ischemic injury have shown limited clinical success1,4,5,9.
Using patient samples of the injured muscle after myocardial infarction and peripheral arterial disease, as well as ischemic mouse muscles, we recently found that macrophages accumulate at perivascular locations11. In the current study, we investigated if the perivascular macrophages in the ischemic muscle acquire a mural cell phenotype and gene expression profile important for re-establishing perfusion. Using two different mouse models of tissue ischemia, in combination with macrophage fate mapping, intravital microscopy and single-cell RNA sequencing (scRNA-seq) analyses, this study demonstrates that macrophages of adult mice can undergo a program to morphologically, transcriptomically and functionally resemble mural cells while downgrading their macrophage identity. The macrophages thereby shift toward a mural cell profile and undertake several mural cell functions important for healing of ischemic injury. This study uncovers an until now unknown role for perivascular macrophages in injured tissue, which may provide a potential target to promote the formation of functional blood vessels in ischemic disease.
Results
Macrophages adopt mural cell characteristics in injured muscle
Macrophages accumulated in the gastrocnemius muscle at day 7 after induction of hindlimb ischemia (HLI) (Extended Data Fig. 1a). Using whole-mount imaging and immunofluorescence, we found that macrophages were located preferentially at perivascular positions where they presented an elongated phenotype mimicking a mural cell-like morphology (Fig. 1a), as previously shown11, and that these macrophages expressed PDGFRβ (Fig. 1a). In fact, the number of macrophages that express the mural cell markers PDGFRβ and neural/glial antigen 2 (NG2) increased significantly at day 7 after ischemia, as determined by flow cytometry of single-cell suspensions from PdgfrβeGFP and Ng2dsRed reporter mice (Fig. 1b). In addition, 91.6 ± 5.4% of PDGFRβ+ macrophages also expressed NG2, as detected by surface staining (Fig. 1b; gating in Extended Data Fig. 1a). To decipher if this observation was due to macrophages upregulating mural cell markers or vice versa, we genetically lineage traced macrophages and studied their response to ischemic injury. For this, Cx3cr1CreERT2 mice were crossed with Rosa26-tdTomato mice, resulting in a heritable expression of tdTomato in myeloid cells including tissue-resident macrophages upon tamoxifen administration (Extended Data Fig. 1b). For simultaneous in situ detection of PDGFRβ expression, the Cx3cr1CreERT2 × Rosa26-tdTomato line was crossed with the PdgfrβeGFP reporter line. Tamoxifen-mediated recombination was followed by a 5 day washout period before induction of HLI to ensure labeling specificity while taking the half-life of tamoxifen and its metabolites into consideration16 (Extended Data Fig. 1c). This approach resulted in 29.3 ± 2.4% and 33.7 ± 4.0% labeled macrophages in circulation and muscle, respectively, assessed at the time of ischemia induction (day 5 of washout; Extended Data Fig. 1d). Characterization of tdTomato+ cells in healthy muscles using flow cytometry (day 5 of washout) showed that the recombined cells are indeed macrophages (Extended Data Fig. 1e). Notably, we also found that PDGFRβ+ cells did not express leukocyte markers before ischemia induction (Extended Data Fig. 1e), validating our lineage tracing strategy.
Consequently, we induced ischemia in mice with lineage-traced macrophages (see Fig. 1c for experimental outline) and found, through in vivo imaging, that tdTomato+ macrophages took on perivascular positions in the ischemic muscle (at day 7 and day 21 after ischemia induction) (Fig. 1d). Approximately 20% of the TdTomato+ cells also expressed GFP (day (D) 7: 20.51 ± 2.54%, D21: 17.78 ± 6.41%), and the tdTomato+PDGFRβ+ cells were found closer to the CD31+ blood vessels when compared to the tdTomato+PDGFRβ− cells at both timepoints (Fig. 1d). Notably, flow cytometry of single-cell suspensions of muscles (gating strategy in Fig. 1e and Extended Data Fig. 1f) revealed that approximately 25–30% of tdTomato+ macrophages downregulated the expression of the myeloid markers CD45 and CX3CR1 (Fig. 1f), whereas 10.3 ± 1.4% and 13.0 ± 1.5% upregulated the mural cell marker PDGFRβ at D7 and D21 after HLI (Fig. 1g), suggesting a macrophage-to-mural cell adaptation in response to ischemia. More than 80% of the lineage-traced cells that expressed PDGFRβ after ischemia induction also expressed NG2 (Fig. 1e; D7: 88.2 ± 2.8%). Immunofluorescent evaluation of tissue sections demonstrated that, 3 weeks after HLI induction, tdTomato+ cells were PDGFRβ+ and were located within the collagen IV+ endothelial basement membrane (Extended Data Fig. 2a), a position shared with pericytes12. Interestingly, although the numbers of PDGFRβ− lineage-traced macrophages were similar before ischemia and at later stages of ischemia onset, PDGFRβ+ lineage-traced macrophages accumulated in ischemic hindlimbs (Fig. 2b). Furthermore, uniform manifold approximation and projection (UMAP) analysis revealed that approximately 20% of the tdTomato+ cells expressed higher levels of PDGFRβ while simultaneously expressing lower levels of several macrophage-associated markers (Extended Data Fig. 2b). In fact, downregulation of several myeloid markers was specifically detected in PDGFRβ+ lineage-traced macrophages, where several of these were further reduced with time (Fig. 1i and Extended Data Fig. 1c,d). Very few lineage-traced macrophages could be detected at 3 months after ischemia induction (319.2 ± 95.6 cells per gram of muscle compared to >10,000 tdTomato+ cells per gram of muscle at D7–D30 after ischemia). Of these, the PDGFRβ+ cells still expressed some macrophage-associated proteins, whereas the PDGFRβ− cells retained only their CD11b expression (Extended Data Fig. 2e). These data demonstrate that macrophages adopt mural cell-like characteristics during the healing phase of ischemic muscle injury….