BACKGROUND
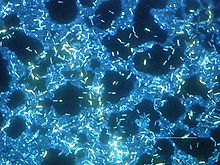
The escalating crisis of multidrug resistance is raising fears of untreatable infections caused by bacterial “superbugs.” However, many patients already suffer from infections that are effectively untreatable due to innate bacterial mechanisms for persistence. This phenomenon is caused by the formation of specialized persister cells that evade antibiotic killing and other stresses by entering a physiologically dormant state, irrespective of whether they possess genes enabling antibiotic resistance. The recalcitrance of persister cells is a major cause of prolonged and recurrent courses of infection that can eventually lead to complete antibiotic treatment failure. Regularly growing bacteria differentiate into persister cells stochastically at a basal rate, but this phenotypic conversion can also be induced by environmental cues indicative of imminent threats for the bacteria. Size and composition of the persister subpopulation in bacterial communities are largely controlled by stress signaling pathways, such as the general stress response or the SOS response, in conjunction with the second messenger (p)ppGpp that is almost always involved in persister formation. Consequently, persister formation is stimulated under conditions that favor the activation of these signaling pathways. Such conditions include bacterial biofilms and hostile host environments, as well as response to damage caused by sublethal concentrations of antibiotics.
ADVANCES
The limited comprehensive understanding of persister formation and survival is a critical issue in controlling persistent infections. However, recent work in the field has uncovered the molecular architecture of several cellular pathways underlying bacterial persistence, as well as the functional interactions that generate heterogeneous populations of persister cells. These results confirm the long-standing notion that persistence is intimately connected to slow growth or dormancy in the sense that a certain level of physiological quiescence is attained. Most prominently, the central role of toxin-antitoxin (TA) modules has been explained in considerable detail. In the model organism Escherichia coli K-12, two major pathways of persister formation via TA modules are both controlled by (p)ppGpp and involve toxin HokB and a panel of mRNA endonuclease toxins, respectively. Whereas activation of the membrane-associated toxin HokB depends on the enigmatic (GTPase) guanosine triphosphatase Obg and causes persister formation by abolishing the proton-motive force, mRNA endonuclease toxins are activated through antitoxin degradation by protease Lon and globally inhibit translation. In addition to these two pathways, toxin TisB is activated in response to DNA damage by the SOS response and promotes persister formation in a manner similar to HokB. Beyond TA modules, many additional factors (such as cellular energy metabolism or drug efflux) have been found to contribute to persister formation and survival, but their position in particular molecular pathways is often unclear. Altogether, this diversity of mechanisms drives the formation of a highly heterogeneous ensemble of persister cells that displays multistress and multidrug tolerance as the root of the recalcitrance of persistent infections.
OUTLOOK
Though recent advances in the field have greatly expanded our understanding of the molecular mechanisms underlying persister formation, important facets have remained elusive and should be addressed in future studies. One example is the upstream signaling input into the pathways mediating bacterial persister formation (e.g., the nature of the pacemaker driving stochastic persister formation). Similarly, it is often not well understood how—beyond the general idea of dormancy—persister cells can survive the action of lethal antibiotics. Finally, one curious aspect of the persister field is recurrent inconsistency between the results obtained by different groups. We speculate that these variations may be linked to subtle differences in experimental procedures inducing separate yet partially redundant pathways of persister formation. It is evident that the elucidation of this phenomenon may not only consolidate progress in the field but also offer the chance to gain insights into the molecular basis and control of bacterial persistence.