Paralysis and sensory deficits are the most obvious consequences of spinal cord injury (SCI). But many people also experience orthostatic hypotension — an inability to maintain blood pressure when moving from lying to sitting or standing1. In the short term, the condition can prevent normal filling of the heart with blood, and can cause light-headedness and dizziness. In the long term, recurrent episodes of orthostatic hypotension increase the incidence of heart attack and stroke, which are leading causes of death in people who have had an SCI. Writing in Nature, Squair et al.2 report a neuroprosthetic strategy that minimizes orthostatic hypotension caused by SCI. The device restores blood-pressure control in rodents, monkeys and humans.
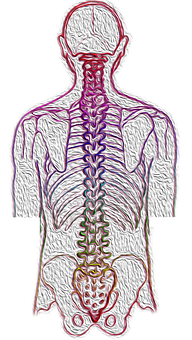
Gravity causes blood to pool in the lower part of the body when we sit or stand. Orthostatic hypotension results mainly from the impairment of reflexes that prevent this pooling. The most crucial of these is the baroreflex, which is initiated by baroreceptors — neurons that sense arterial blood pressure and the degree of filling of the large veins and heart chambers3. In mammals, these sensors are active when the body is at rest. A reduction in arterial blood pressure or blood volume reduces baroreceptor activity. This, in turn, activates the sympathetic branch of the autonomic nervous system, restoring blood pressure by increasing vascular resistance and the flow of blood back to the heart4. SCI interrupts the connection between the lower brainstem, which receives the information from the baroreceptors, and the sympathetic neurons that innervate the cardiovascular system, which originate from thoracic and upper lumbar spinal segments (Fig. 1).
Orthostatic hypotension is typically managed by lifestyle changes (such as using compression bandages on the legs and sleeping in a semi-upright position) and drugs such as fludrocortisone (a blood-volume expander) or midodrine (which activates the receptors that normally mediate the effect of the sympathetic nerves on the heart and vascular muscles)5,6. However, these drugs can have untoward effects. Other approaches include electrical stimulation of skeletal muscles in the lower limbs, which activates the muscle pump and aids cardiac filling, and abdominal constriction belts. Both of these strategies have been used therapeutically, but their effectiveness has not been clearly demonstrated6.
Could neuroprosthetic devices be a better alternative? The principle is to restore function by electrically stimulating the neural pathways that have become unresponsive as a result of SCI. Ideally, the stimulation should closely approximate the pattern of activity that normally controls the targeted function. Such an approach has already been used to partially restore locomotion in primates7. It has also been used to activate the leg muscles to improve blood-pressure control in people with an SCI8, although the reasons for its apparent success in this setting were unclear….