Abstract
Bacteriophages are ubiquitous viral predators that have primarily been studied using fast-growing laboratory cultures of their bacterial hosts. However, microbial life in nature is mostly in a slow- or non-growing, dormant state. Here, we show that diverse phages can infect deep-dormant bacteria and suspend their replication until the host resuscitates (“hibernation”). However, a newly isolated Pseudomonas aeruginosa phage, named Paride, can directly replicate and induce the lysis of deep-dormant hosts. While non-growing bacteria are notoriously tolerant to antibiotic drugs, the combination with Paride enables the carbapenem meropenem to eradicate deep-dormant cultures in vitro and to reduce a resilient bacterial infection of a tissue cage implant in mice. Our work might inspire new treatments for persistent bacterial infections and, more broadly, highlights two viral strategies to infect dormant bacteria (hibernation and direct replication) that will guide future studies on phage-host interactions.
Introduction
Unlike the rapidly dividing cells that may come to mind at first when thinking of microbes, most bacteria on our planet are in a slow- or non-growing, dormant state characterized by a low-energy physiology and high resilience to external perturbations1. This includes completely inactive spores—described as “the purest form of microbial dormancy”—but also a wide variety of quiescent yet vigilant states of low activity that are poised to resuscitation when nutrients or signaling molecules are supplied2,3,4. These dormant bacteria are usually seen as a microbial bet-hedging strategy to ensure population survival via the persistence of heterogeneous, highly resilient cells through unpredictable catastrophic events5. In many cases, bacterial dormancy is induced through a well-ordered physiological program in response to stress or starvation that also controls the “stationary phase” of laboratory cultures after exhausting the growth potential of their culture conditions1,6. For the model organisms Escherichia coli and Pseudomonas aeruginosa, these processes are largely orchestrated by signaling through the stress and starvation sigma factor RpoS as well as the second messenger (p)ppGpp1,6,7,8,9.
The antibiotic drugs administered in clinics constitute just another unpredictable existential threat that bacteria can evade through dormancy. While antibiotic resistance denotes the ability of bacteria to grow in presence of an antibiotic, the antibiotic tolerance of dormant cells causes a slower killing compared to growing cells because the cellular processes commonly poisoned by bactericidal antimicrobials are tuned down or inactive10,11,12. Therefore, dormant antibiotic-tolerant cells sometimes known as “persisters” can survive drug treatment and have been implicated in the resilience of chronic or relapsing infections13. Despite decades of intensive research, common underlying principles of these heterogeneous persister cells are still hotly debated and no effective treatments are available in clinics10,11,12. While new antimicrobials from classical in vitro research might help us fight antibiotic-resistant infections, they are likely to be as ineffective against antibiotic persistence in vivo as the regular antibiotic drugs that are currently available.
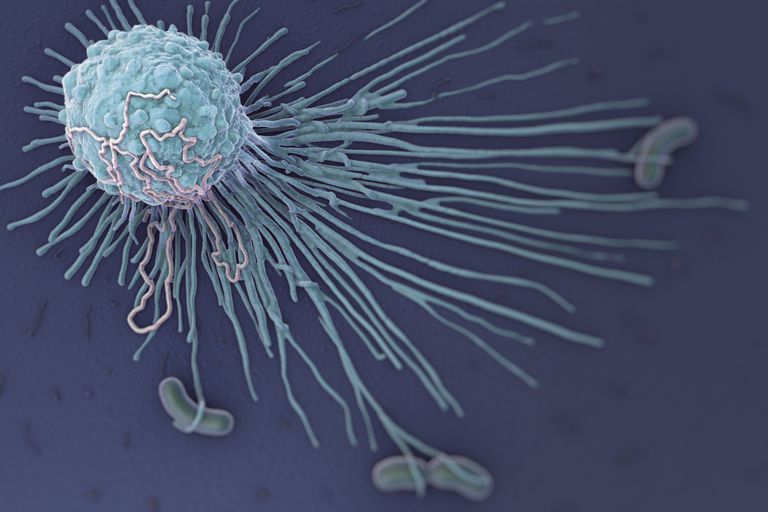
One promising alternative strategy to combat antibiotic resistance is the therapeutic application of bacteriophages (or short “phages”), the viruses that prey on bacteria14,15. Despite its long history, phage therapy has remained a niche approach in most countries due to technical difficulties and a notorious lack of reliability in clinical trials14,15. Already almost hundred years ago a dedicated study concluded that “the bacteriophage, which acts so well in vitro, does not have a similar action in vivo16”. The physiology of bacteria at the infection site is therefore a key parameter for phage infectivity and, consequently, for successful phage therapy, but the underlying molecular mechanisms are only poorly understood17,18,19,20. Analogous to antibiotic persistence, it is intuitive that the dormancy of stressed and starved bacteria in vivo might impair phage therapy. Previous work indeed showed that the productivity of phage infections is positively correlated with host growth rate and that fully growth-arrested cells are refractory to phage replication21,22,23,24,25.
Consequently, commonly studied virulent phages either avoid adsorption to dormant bacteria26 or hibernate in the low-energy physiology of these cells until nutrients become available again and lytic replication resumes25,27,28,29. The latter phenomenon is known as pseudolysogeny30 analogous to the lysogeny of temperate phages which can integrate their genome into the host’s genome, e.g., when they encounter starved host cells31. Nevertheless, we reasoned that phages with the ability to directly replicate on dormant hosts likely exist in nature given the abundance and diversity of dormant bacteria and the density of phage-host interactions1,32. Previous work indeed described a few examples of phages with this ability33,34,35 and reported cases of successful phage therapy targeting chronic bacterial infections20,36,37. However, the underlying molecular mechanisms and possible phage replication on truly deep-dormant, antibiotic-tolerant bacteria had remained elusive. Studying such phages would give important insights into viral ecology in nature and might open new avenues to treat chronic infections, e.g., by inspiring new treatment strategies to overcome the resilience of dormant bacteria.
In this study, we therefore performed large-scale bacteriophage isolation experiments to isolate new phages with the ability to directly kill antibiotic-tolerant, dormant cells of Escherichia coli or Pseudomonas aeruginosa by lytic replication. While most phages seemed to merely hibernate in these hosts, we isolated a new P. aeruginosa phage named Paride that uniquely replicates on deep stationary-phase cultures of laboratory and clinical strains of this organism. Intriguingly, we found that Paride can even sterilize deep-stationary phase cultures of P. aeruginosa if combined with the β-lactam meropenem via a phage-antibiotic synergy that also strongly reduces bacterial loads in a murine tissue cage infection model. Unexpectedly, the replication of Paride on dormant hosts largely depended on the bacterial starvation and stress response signaling that is also required for the antibiotic tolerance of these bacteria. This suggests that Paride specifically exploits weak spots in the resilient physiology of dormant bacteria that could be targeted as Achilles’ heels by new treatment options.
Results
Commonly studied bacteriophages can’t replicate on antibiotic-tolerant, deep-dormant bacteria
We initiated our study by exploring the ability of multiple different phages including commonly used laboratory models to kill deep-dormant cultures of Escherichia coli or P. aeruginosa by direct replication. Given that well-chosen and strictly controlled assay conditions are crucial for meaningful experiments with dormant bacteria10,12,38,39, we had previously established a rigorous methodology that is based on a fully defined culture medium and enables work with both growing or non-growing, stationary phase bacteria40. In the current study, we have now performed whole-proteome analyses of these cultures during rapid growth and at different time points in stationary phase to further characterize our experimental system (see “Methods”). Briefly, our results confirmed the intuitive notion that the bacterial physiology shifts massively when growth stalls upon entry into stationary phase ca. 8 h after subculturing40 and then continues to change from this state of early dormancy while the bacteria become more starved and stressed until deep dormancy 48 h after subculturing (Fig. S1). To study antibiotic tolerance or phage sensitivity, bacterial cultures were then challenged with drugs and/or viruses during exponential growth or in a deep-dormant state (48 h after subculturing/ca. 40 h after entering stationary phase) and bacterial viability as well as viral infections were tracked over time40 (Fig. 1a).
In this setup, fast-growing cultures of E. coli and P. aeruginosa are readily cleared by antibiotic treatment and highly permissive to replication by all tested bacteriophages (Fig. 1b). Conversely, the deep-dormant cultures displayed massive antibiotic tolerance and did not allow replication of any tested bacteriophage (Fig. 1c–e). Instead, most phages rapidly adsorbed and then seemed to enter a state of hibernation in dormant hosts that is apparent as a stable number of infected cells over time as observed already previously, e.g., for E. coli phage T4 and P. aeruginosa phage UT128,29.
Previous studies had highlighted the ability of E. coli phage T7 to replicate on starved, stressed, and stationary phase hosts33,41, but we merely observed hibernation of this phage when infecting deep-dormant cultures (Fig. 1c). Given the exceptionally long cultivation of bacteria in our setup before phage or antibiotic challenge, we suspected that the host cells in previous work might have been in a less dormant and, consequently, more permissive physiological state. To test this hypothesis, we generated analogous data using early stationary phase cultures treated either 8 h after subculturing (when cultures have just reached maximal density40) or 4 h later. As expected, the bacteria at these time points displayed an intermediate antibiotic tolerance that was higher than for growing cells but lower than our deep-dormant cultures treated 48 h after subculturing (Fig. 2a as well as S2a–c and S3a, b). Intriguingly, phage T7 stood out from all other tested E. coli and P. aeruginosa phages for its ability to replicate on the cultures treated 8 h after subculturing while no phage could replicate on the bacteria challenged 12 h after subculturing (Fig. 2a as well as S2a–c and S3a, b). These results confirm a special ability of phage T7 to replicate on some stressed and starved cells that exhibit intermediate antibiotic tolerance but clearly showed that highly drug-tolerant, deep-dormant cells were off limits for all previously tested phages.
Bacteriophage Paride can kill deep-dormant P. aeruginosa by direct lytic replication
To isolate new phages that could replicate on these cells, we therefore resorted to the systematic screening of environmental samples using deep-dormant cultures of E. coli or P. aeruginosa as bait (see “Methods”). These experiments resulted in the isolation of bacteriophage Paride, a P. aeruginosa phage that rapidly adsorbs to deep-dormant host cells and then massively replicates, killing >99% of the bacterial population and causing the culture to lyse (Figs. 2b and S3c). Interestingly, Paride also proficiently replicates on growing host cells (Fig. S3d). The phage forms virions of myovirus morphotype and has a large genome of 287,267 bp, i.e., far beyond the 200 kb threshold defining “jumbo phages” (NCBI GenBank accession OR805295; Fig. 2c)42. Phylogenetic analyses revealed that Paride is a close relative of previously described phages PA5oct and MIJ3 (Fig. 2d)43,44. Conversely, Paride is not related to well-studied P. aeruginosa jumbo phage phiKZ which famously forms a “phage nucleus” in infected cells45 but cannot replicate on dormant hosts (Figs. 1c and S3a, b), and belongs to an entirely different clade of large microbial viruses42.
Repeated attempts at isolating different phages that can replicate on deep-dormant, antibiotic-tolerant bacteria exclusively uncovered diverse close relatives of Paride that we called Cassandra, Deifobo, and Ettore (Fig. 2d and Table S1) but no other phage, suggesting that this ability is very rare. We therefore explored whether the observed replication of Paride on deep-dormant cultures might be a laboratory artifact from the combination of this phage and the P. aeruginosa PAO1 model strain. However, Paride also readily replicated on stationary-phase cultures of different susceptible P. aeruginosa strains from a collection of clinical isolates (Figs. 3a, b and S4a), demonstrating that this phenomenon is not restricted to the PAO1 laboratory strain….