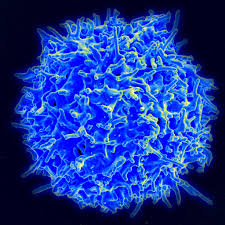
In May, researchers showed that people with mild forms of COVID-19, the disease caused by the SARS-CoV-2 virus, have circulating T cells that respond to the virus. Now, in a Science Immunology study published last week (June 26), a collaborating research team has determined that people who are sick enough with COVID-19 to be hospitalized in the intensive care unit also make SARS-CoV-2-reactive T cells. In both studies, the researchers found that a subset of healthy, unexposed people also had some of these T cells that react to the virus, perhaps due to previous exposures to other coronaviruses that cause symptoms of the common cold.
The latest study provides more solid evidence that there are SARS-CoV-2-specific T cells that are induced by the infection, says Antonio Bertoletti, who studies T cells at Duke-NUS Medical School in Singapore and was not involved in the work. This is important because researchers have put a lot of emphasis on antibodies, he adds, but it’s still not clear whether antibodies or T cells are more important for protection from the virus.
Rory de Vries, a virologist and immunologist at Erasmus University Medical Center in the Netherlands, was visiting immunologist Alessandro Sette’s lab at the La Jolla Institute for Immunology in California to collaborate on another project when “all hell broke loose” with the pandemic, Sette tells The Scientist. Sette’s group had been developing tools to investigate adaptive immunity to SARS-CoV-2, but in California at that point, they didn’t have a COVID-19 patient population to try them in. As de Vries prepared to return home in March, Europe already had confirmed cases of SARS-CoV-2, so he took the tools the team had developed back to the Netherlands.
de Vries and colleagues collected blood from 10 COVID-19 patients—four women and six men admitted to the intensive care unit with acute respiratory distress syndrome requiring ventilation—and 10 healthy volunteers. The team exposed the study participants’ immune cells to a pool of predicted SARS-CoV-2 peptides in vitro to see whether or not the cells would react.
The team determined that all of the ill patients had fewer overall T cells than the healthy volunteers, which was consistent with earlier findings from other groups. All patients had helper T cells and eight of 10 had killer T cells that targeted SARS-CoV-2 proteins. These reactive T cells showed up within about 10 days of symptom onset in the patients. The strongest responses were to the SARS-CoV-2 spike protein, but cells responded to membrane and nuclear viral proteins, too….