As of today (January 23), 18 people have died from a newly identified coronavirus, and more than 630 have been infected. Airports are screening passengers coming from at-risk regions. Public celebrations of the Lunar New Year have been cancelled in several Chinese cities. China has stopped trains and other transportation leaving Wuhan, where the infections originated, and restricted travel within the city and neighboring areas. The World Health Organization (WHO) held a conference today to discuss the travel bans and other precautions related to the new disease, currently being called 2019-nCoV, a respiratory virus with characteristics similar to severe acute respiratory syndrome (SARS) from 2003.
As public health officials respond in real-time to the unfolding of the outbreak, so too are scientists. Just one month after the first case of the pneumonia-causing virus was reported on December 8, Chinese scientists sequenced the viral genome and made it public. Now, researchers around the globe are scrutinizing the sequence for insight into this mystery disease.
“It really is an amazing feat that they got these sequences out as quickly as they did,” says Vineet Menachery, a virologist at the University of Texas Medical Branch who has studied the new genome. That speed, he notes, stands in contrast with the SARS outbreak, in which “for many months, it was not known that there was an outbreak.”
While there are still concerns that China has silenced critics and downplayed the seriousness of the disease, the genome’s availability is already helping doctors properly diagnose the infection. It causes flu-like symptoms such as cough and fever that make it difficult to distinguish from other, more common illnesses.
“It seems like it might be a little less clinically severe than SARS, though it’s still very early,” says Alex Greninger, a virologist at the University of Washington. “This virus has escalated quite quickly. And when you’re at this point in the epidemic curve, it’s very hard to know which way things are going.”
When a man in Washington state developed mild symptoms two days after returning from Wuhan on January 15, his doctors shipped his sample overnight to the US Centers for Disease Control and Prevention, which used real-time reverse transcription polymerase chain reaction (rRT-PCR) to confirm that the sample matched the genetic sequence of 2019-nCoV. The strategy can also be used to determine the presence of the virus in individuals who don’t show symptoms but may still be able to spread it to others. Without the genome, officials would not have been able to definitively diagnose the disease.
The virus is somewhat similar to the SARS virus, says Menachery. He points out that almost all of 2019-nCoV’s proteins are the same as SARS’s, but “it does have differences in the key areas that you would expect will influence its ability to infect humans.”
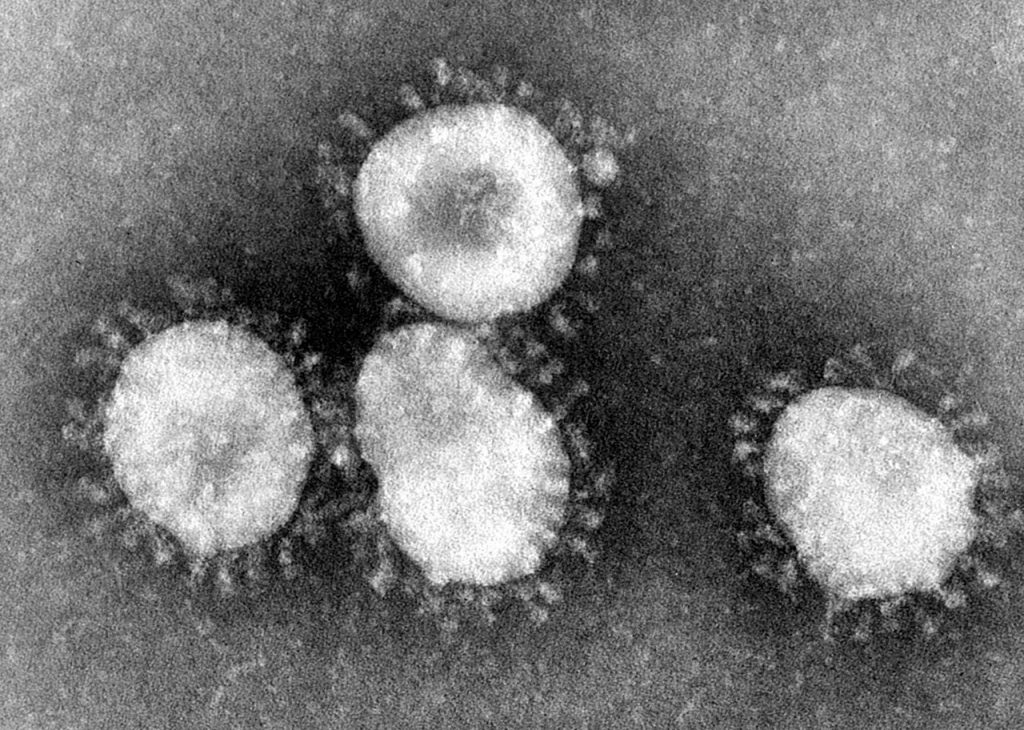
Coronaviruses are so named because they have surface proteins that stick out like tips on a crown. These spikes help them invade cells. The S1 region of the protein first binds to a receptor on a human (or animal) cell, and the S2 region then fuses and allows the virus to enter that cell. Menachery says the S2 portion of the spike protein on the coronavirus matches that of the SARS virus, but the S1 region is somewhat different, meaning 2019-nCoV could use a different cell receptor for entry than the SARS virus does. However, a preprint that came out today from Wuhan-based scientists suggests that the two viruses do, in fact, utilize the same cell entry receptor, ACE2.
It’s possible that antiviral treatments currently in development to treat other viruses may be able to treat this new virus. The genomic analysis has suggested that the virus’ RNA polymerase—the target of one such drug called remdesivir—is conserved in 2019-nCoV. “We’d expect that they would work. But again, you don’t know that they’ll work until you actually test them. Nature has a way of getting around things,” says Menachery. Plus, the treatments haven’t been approved for any indications yet. There is a clinical trial recruiting patients to test the drug’s ability to treat Ebola, but other work is still preclinical.
Some of the most important characteristics of the disease can’t be understood from the virus’ genome alone. It was only earlier this week that researchers determined the virus could spread between humans and did not require direct contact with an infected animal. Researchers still aren’t sure how it is transmitted between people. “Is it shed only in respiratory secretions? Is it found in the urine? Is it found in the blood? Is it found in stool? What’s infectious? How long’s it infectious? How high the viral load can get,” says Greninger, “all those things are enabled by the genome, certainly. But you can’t deduce it from the genome.”
Additionally, while scientists know the virus emerged in Wuhan, China, at a market known for selling all sorts of live animals from both land and ocean, it’s unclear what species the virus came from, and that can’t be determined from the genome alone. “Knowing the source of the SARS epidemic really helped stamp out the problem,” says Anthony Fehr, who studies coronaviruses at the University of Kansas. “We can’t figure out the source just knowing the [genetic] sequence.”
The genome does give scientists some insight, though. For example, there was very little genetic variation between the first 10 patient samples sequenced by various teams across the world. Menachery says that’s a sign the virus recently jumped from animals to humans. “It doesn’t appear that these viruses have been in human populations for a long time and just not recognized,” he says. “It appears that they potentially recently emerged from either an animal host or some other location.”
Scientists will need to keep comparing new samples to determine how the virus adapts as it infects more people. “The other thing the sequence allows us to do,” says Fehr, “is see if the virus is evolving in real time. Are there mutations in the virus adapting to the human population; is it becoming more easily transmitted between humans because of certain mutations?”
On January 22, a team of China-based scientists published an article based on the virus’ genome that suggested it’s possible the coronavirus emerged from snakes. But, “the paper does not provide direct evidence that this virus was transmitted to humans from snakes and the indirect evidence is tenuous at best,” says Mark Stenglein, a virologist at the University of Colorado, in an email to The Scientist. “Scientists should disseminate only well supported information, especially in the context of a possible public health emergency.”
Only about 2 percent of those infected with the new coronavirus have died. So far, those deaths have primarily been older men with preexisting conditions, but many more have ended up seriously ill and are still in the hospital, according to officials at the WHO conference today. “In the next couple of weeks or so, we’re going to see more and more cases. We’re going to start to see how serious it really is,” says Peter Gulick, an infectious disease specialist at Michigan State University. “Right now, we’re just hearing numbers here, numbers there . . . numbers that may not have substance, but just may make you worry.”