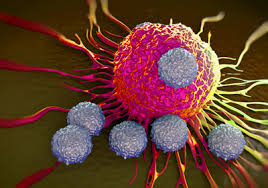
Immune cells called CD8 (or cytotoxic) T cells can target and kill cancer cells, and immunotherapies that boost this process are in clinical use. However, for reasons that are not fully clear, it is hard to predict whether a person will respond to this treatment. Writing in Nature, Alspach et al.1 report mouse studies revealing that another type of immune cell, called a CD4 cell (also known as a helper T cell), has a crucial role in aiding CD8 T cells to target tumours after immunotherapy.
Mutations in tumour cells can give rise to abnormal proteins, fragments of which — termed neoantigens — are displayed on the surface of cells bound to major histocompatibility complex (MHC) molecules. If a neoantigen is recognized by a CD8 T cell, this cell can target and kill any tumour cells that express the neoantigen. However, this cytotoxic response can be blocked, for example by an immunosuppressive environment surrounding a tumour. Immunotherapy treatments called immune-checkpoint blockade or immune-checkpoint therapy can counteract such problems to enable CD8 T cells to unleash an effective immune response against the tumour.
Much immunotherapy research focuses on CD8 T cells. However, there is emerging evidence that CD4 T cells might have a key role in tumour-targeting immune responses2,3.
Alspach and colleagues sought to identify the minimal immune-stimulating neoantigen requirement to drive an effective immune response in mice that were given an immunotherapy treatment. The authors studied mice that had a type of tumour to which the immune system does not normally respond, and they engineered such tumours to express neoantigens. The neoantigen termed mLAMA4 is recognized by CD8 T cells4, and the neoantigen termed mITGB1, recognized by CD4 T cells, was identified by the authors using a computational prediction method. In the absence of immunotherapy, the expression of these two neoantigens, either alone or together in a tumour, was insufficient to trigger an effective immune response against the tumour. However, if both neoantigens were expressed in animals receiving immunotherapy, the tumour regressed.
To check whether this response was simply dependent on neoantigen quantity, rather than the need for neoantigen recognition by both types of immune cell, the authors engineered mouse tumours to express two different neoantigens that are recognized by CD8 T cells, but not by CD4 cells. These tumours did not respond to immunotherapy, demonstrating that a successful immune response depends on the presence of neoantigens that trigger responses from both CD4 and CD8 T cells.
The authors’ analysis reveals that the CD4 T cells that responded to mITGB1 had the hallmarks of a type of CD4 T cell called a T helper type 1 cell, which can increase the number and cell-killing activity of CD8 T cells2. The authors confirmed that, if tumours expressed both mLAMA4 and mITGB1, this indeed caused an increase in the number and cytotoxic activity of CD8 T cells, compared with the case for animals with tumours that expressed only mLAMA4. Alspach and colleagues also showed that, if animals were first vaccinated with dying tumour cells and were then implanted with a growing tumour that expressed mLAMA4 and mITGB1, the transplanted tumours were most efficiently rejected if the vaccine contained tumour cells that expressed both mLAMA4 and mITGB1 in the same cell…