It’s another sign that an era of untreatable bacterial infections is inching closer. Today, the World Health Organization (WHO) released new guidelines for treating gonorrhea that reflect the sobering reality that this sexually transmitted disease is becoming ever more difficult to treat. WHO recommends no longer using quinolones, a class of antibiotics that has become less and less effective. And for the first time, the agency makes suggestions on what to do when none of the standard drugs work.
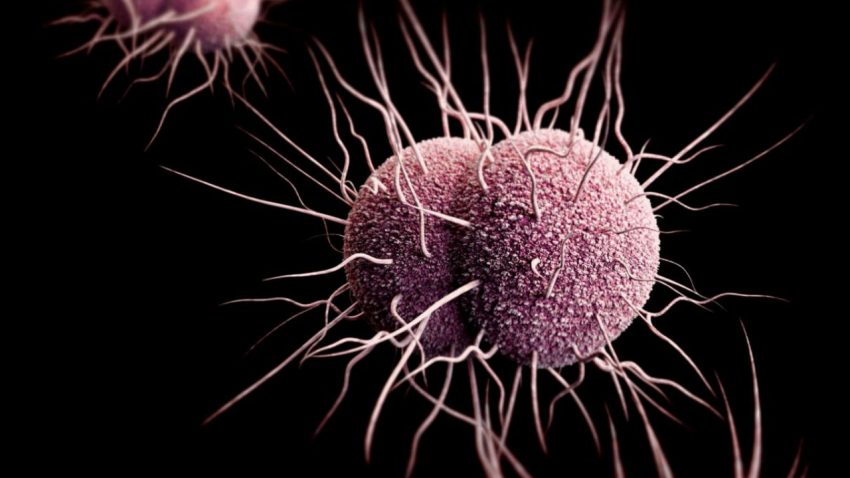
Gonorrhea, caused by the bacterium Neisseria gonorrhoeae, infects an estimated 78 million people every year. Although many suffer no symptoms, the bacterium can cause pain in the genitals, rectum, and throat, and can lead to infertility and infections of the brain or the heart if untreated. Current WHO guidelines, written in 2003, recommend treating infections with quinolones, such as ciprofloxacin. But resistant strains of the bacterium have now spread across the globe, says Teodora Wi from WHO’s Department of Reproductive Health and Research in Geneva, Switzerland, making quinolones all but useless. Another class of drugs called cephalosporins should be the first line of defense.
Many high-income countries changed their guidelines years ago based on their own data. But WHO’s guidelines set a global standard and are particularly important for low-income countries that do not have good surveillance data. “We really wanted countries to remove quinolones as the treatment of choice,” Wi says. “Imagine if African countries invest so much money just to buy quinolones and the bacteria are already resistant.”
Cephalosporins, including a widely used drug named ceftriaxone, have their problems as well. Forty-six countries have reported gonorrhea strains with decreased susceptibility to ceftriaxone, and 10 have reported patients for whom none of the usual antibiotics were effective, Wi says. “We risk losing the last antibiotic class for the effective treatment of gonorrhea,” says Vanessa Allen, chief of medical microbiology at Public Health Ontario in Toronto, Canada.
Even when cephalosporins fail, doctors have some options left. The new guidelines suggest trying combinations of drugs, including older antibiotics like gentamicin and spectinomycin. But those have been studied less and N. gonorrhoeae is known to develop resistance against them very quickly. WHO is looking at initiatives to develop new gonorrhea drugs, Wi says. “We will have to have new drugs in 5 years, I think.”
The few alternatives to antibiotics are very unattractive. Before penicillin became available in the middle of the 20th century, patients with gonorrhea often had to endure painful treatments in the hospital. “Mechanical interventions included genital installation of large quantities of iodine solution instilled by urethral or vaginal catheters, or ‘hot boxes’ where a person’s body was put in a box to 43°C to try to kill off the organism and not the host,” Allen says. “A return to this preantibiotic era is becoming an increasing possibility unless we slow down the rate of resistance or develop new drugs soon enough.” Treatment guideline changes in the United Kingdom and Canada led to a decrease in resistance, Allen says. “But we will have to see what this will do on an international scale.”
WHO also revised guidelines for treating chlamydia and syphilis, two other important sexually transmitted infections for which resistance is less of a problem. A single dose of benzathine penicillin, for instance, is still considered the best option to cure syphilis. But there is a shortage of that drug, Wi says: “It is so cheap that many companies don’t want to manufacture it.” WHO is working on addressing the issue, she says. Syphilis is particularly dangerous in pregnant women, who can transmit the disease to their fetus, leading to an estimated 143,000 miscarriages and 62,000 deaths among newborn babies every year.