Highlights
- •Transcriptional-translational conflict is tumor suppressive in bladder epithelium
- •De-repression of translation elongation enables oncogenic phenotypes
- •ARID1A-low tumors are sensitive to drug-induced transcriptional-translational conflict
- •Impaired DNA damage response is a collateral effect of gene expression conflict
Summary
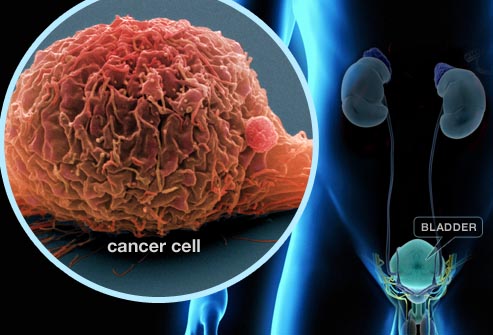
We uncover a tumor-suppressive process in urothelium called transcriptional-translational conflict caused by deregulation of the central chromatin remodeling component ARID1A. Loss of Arid1a triggers an increase in a nexus of pro-proliferation transcripts, but a simultaneous inhibition of the eukaryotic elongation factor 2 (eEF2), which results in tumor suppression. Resolution of this conflict through enhancing translation elongation speed enables the efficient and precise synthesis of a network of poised mRNAs resulting in uncontrolled proliferation, clonogenic growth, and bladder cancer progression. We observe a similar phenomenon in patients with ARID1A-low tumors, which also exhibit increased translation elongation activity through eEF2. These findings have important clinical implications because ARID1A-deficient, but not ARID1A-proficient, tumors are sensitive to pharmacologic inhibition of protein synthesis. These discoveries reveal an oncogenic stress created by transcriptional-translational conflict and provide a unified gene expression model that unveils the importance of the crosstalk between transcription and translation in promoting cancer.
Introduction
Major tumor suppressors such as TP53, PTEN, APC, and PDCD4 are negative regulators of mRNA translation. Downregulation of each gene leads to an increase in mRNA-specific translation through cap-dependent and cap-independent mechanisms enabling cancer pathogenesis.1,2,3,4 These findings suggest that a major function of tumor suppression is to downregulate the protein abundance of oncogenic gene networks. Recently, pan-cancer genome sequencing coupled with mechanistic work has uncovered a new class of tumor suppressors involved in chromatin remodeling.5,6,7,8 In particular, components of ATP-dependent SWI/SNF family nucleosome remodeling complexes are mutated in 20% of human cancers.9 Of these, the defining component of the BAF ATP-dependent SWI/SNF nucleosome remodeler called AT-rich interactive domain-containing protein 1A (ARID1A) is the most frequently mutated.10 ARID1A is considered a tumor suppressor because genetic deletion leads to the transcriptional activation of oncogenic mRNAs, impairments in double-stranded DNA break repair and decatenation, and tumor progression.5,6,7,11,12 It remains to be determined how ARID1A regulates protein synthesis in normal tissues.
We uncover a relationship between ARID1A and mRNA translation that challenges the prevailing dogma that tumor suppressors inhibit protein synthesis and introduces a tumor-suppressive process in urothelium called transcriptional-translational conflict. Although deletion of Arid1a promotes the transcription of a regulon of potentially oncogenic genes, this is countered by a paradoxical decrease in translation elongation rates. The resulting transcriptional-translational conflict specifically restrains the synthesis of pro-proliferation and mitogenic proteins and collateral DNA damage response (DDR) genes thereby preventing uncontrolled cell growth and cancer progression. Restoring translation elongation rates is needed to drive the tumor promoting properties of ARID1A loss. Remarkably, ARID1A-null tumors retain a memory of this translational dependence, which represents a selective therapeutic vulnerability. These findings reveal an oncogenic stress created by transcriptional-translational conflict that is a gatekeeper of urothelial homeostasis.
Results
Loss of Arid1a leads to a gene-specific transcriptional-translational conflict in urothelium
To study the physiologic impact of deleting Arid1a on gene expression, we used a UBC-CreERT2;ROSA-LSL-YfpKI/KI;Arid1aLoxP/LoxP mouse model (herein referred to as Arid1afl/fl) in which the administration of tamoxifen leads to deletion of ARID1A and expression of YFP in multiple tissues (Figure 1A). Within the urothelium, we observed a recombination efficiency of 83% (Figure S1A). We focused on the urothelium because bladder cancer is the 6th most common malignancy in humans,13 and 25% of urothelial carcinoma patients exhibit Arid1a loss-of-function mutations.14,15,16 Given that Arid1a loss has been shown to increase transcript levels of oncogenic genes in other tissues,5 we sought to determine if the same is true within urothelial cells. We isolated basal cells, a cell of origin of invasive urothelial malignancies,17,18 from wild-type (WT) and Arid1afl/fl bladders and conducted RNA sequencing (RNA-seq) (Figure S1B). We observed 262 upregulated mRNAs in Arid1afl/fl cells, and 80% of these were direct targets of Arid1a (Figure S1C; Table S1). Most overexpressed mRNAs were classified as regulators of cell proliferation (Figure 1B). Furthermore, these genes included aurora kinase B (Aurkb), insulin-like growth factor 2 (Igf2), fibroblast growth factor receptor 3 (Fgfr3), and ornithine decarboxylase 1 (Odc1), all of which are cancer drivers (Figure 1C).19,20,21,22 Overexpression of Aurkb, Igf2, or Fgfr3 in transgenic models is sufficient to drive uncontrolled cell growth and tumor formation.23,24,25 Given these findings, we subsequently aged Arid1afl/fl mice for 400 days to determine if they develop bladder tumors. Despite the transcriptional activation of these gene networks, Arid1afl/fl mice exhibited a decrease in urothelial thickness characterized by fewer basal cells, and 0 of 9 mice developed tumors (Figure 1D).