Abstract
Trastuzumab deruxtecan (T-DXd) intracranial activity has been observed in small or retrospective patient cohorts with human epidermal growth factor receptor 2–positive (HER2+) advanced/metastatic breast cancer (mBC) and stable or active (untreated/previously treated and progressing) brain metastases (BMs). The phase 3b/4 DESTINY-Breast12 study investigated T-DXd in patients with HER2+ mBC and is, to our knowledge, the largest prospective study of T-DXd in patients with BMs in this setting. Patients (stable/active BMs (n = 263) and no BMs (n = 241)) treated with one or more prior anti-HER2–based regimens received T-DXd (5.4 mg per kg). Primary endpoints were progression-free survival (PFS; BMs cohort) and objective response rate (ORR) per Response Evaluation Criteria in Solid Tumors version 1.1 (non-BMs cohort). Additional endpoints included central nervous system (CNS) PFS, ORR, time to second progression, CNS ORR (BMs cohort), incidence of new symptomatic CNS metastases (non-BMs cohort), time to progression, duration of response, overall survival and safety (both cohorts). No formal hypothesis testing was conducted for this single-arm, open-label study. In the BMs cohort, 12-month PFS was 61.6% (95% confidence interval (CI): 54.9–67.6), and 12-month CNS PFS was 58.9% (95% CI: 51.9–65.3). In the non-BMs cohort, ORR was 62.7% (95% CI: 56.5–68.8). Grade 3 or higher adverse events occurred in 51% (BMs cohort) and 49% (non-BMs cohort) of patients. Investigator-reported interstitial lung disease/pneumonitis occurred in 16% (grade ≥3: 3%) of patients with BMs and 13% (grade ≥3: 1%) of patients without BMs. These data show substantial and durable overall and intracranial activity for T-DXd, supporting its use in previously treated patients with HER2+ mBC irrespective of stable/active baseline BMs. ClinicalTrials.gov identifier: NCT04739761.
Main
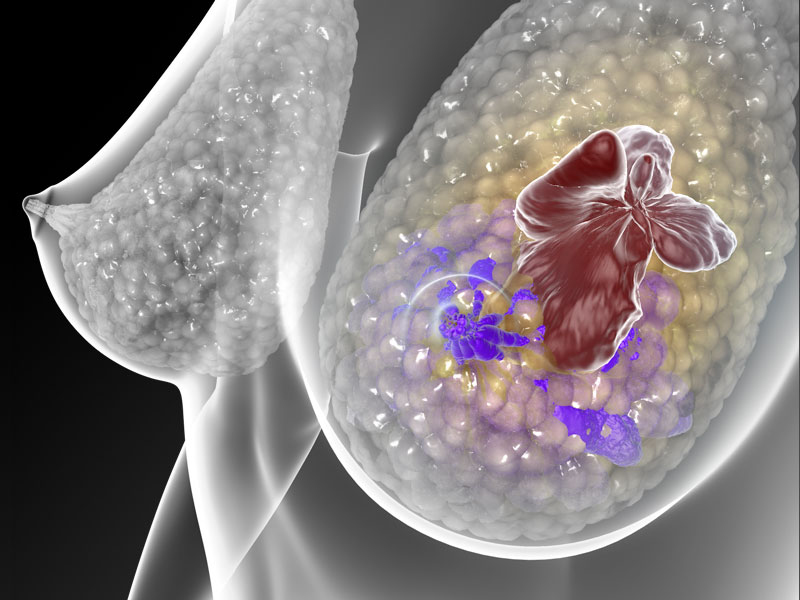
Human epidermal growth factor receptor 2–positive (HER2+) breast cancer accounts for between 15% and 20% of all cases of breast cancer1,2. As many as 50% of patients with HER2+ advanced/metastatic breast cancer (mBC) develop brain metastases (BMs), which are associated with a poorer prognosis compared to patients who do not have BMs3,4,5,6.
Local therapy (including surgical resection, stereotactic radiosurgery (SRS), stereotactic radiotherapy and/or whole-brain radiation therapy (WBRT)) is recommended for BMs7; however, central nervous system (CNS) progression typically occurs within 6–12 months of treatment, and no extracranial benefit is conferred8,9,10,11. WBRT, currently recommended for treatment of multiple BMs, is associated with cognitive deterioration7,12; as some patients with HER2+ breast cancer and BMs can survive for several years, this is of particular concern13. As such, additional systemic treatment options for patients with BMs are needed. Trastuzumab-based therapy has long been the mainstay of systemic therapy for patients with HER2+ mBC, and several additional HER2-directed therapies have been investigated for the treatment of HER2+ mBC with BMs, including tucatinib14,15,16,17. Despite this, a large proportion of patients receiving treatment, including those with an initial response, eventually experience disease progression (commonly in the CNS)17.
Trastuzumab deruxtecan (T-DXd) is an antibody–drug conjugate (ADC) composed of a humanized immunoglobulin G1 monoclonal antibody specifically targeting HER2, a tetrapeptide-based cleavable linker and a potent topoisomerase I inhibitor payload18,19. On the basis of results from the randomized phase 3 DESTINY-Breast03 study, T-DXd is approved for the treatment of adult patients with unresectable or metastatic HER2+ breast cancer who have received a prior anti-HER2–based regimen in the metastatic setting or who have received a prior anti-HER2–based regimen in the neoadjuvant or adjuvant setting and developed disease recurrence during or within 6 months of completing therapy20,21.
Promising preliminary evidence of T-DXd intracranial efficacy was reported in a retrospective, exploratory pooled analysis of DESTINY-Breast01, 02 and 03. Patients with HER2+ mBC and stable (n = 104) or active (n = 44) BMs were treated with T-DXd22. The intracranial objective response rate (ORR) was 45.2% in patients with stable BMs and 45.5% in patients with active BMs. Median (95% confidence interval (CI)) CNS progression-free survival (CNS PFS) was 12.3 months (11.1–13.8) in patients with stable BMs and 18.5 months (13.6–23.3) in patients with active BMs22. Encouraging intracranial responses in patients with active (untreated or previously treated and progressing) BMs were also reported in the phase 1b/2 DESTINY-Breast07 study (n = 35); in the ongoing, five-cohort phase 2 DEBBRAH study (n = 13); in ROSET‑BM, a multicenter, retrospective, medical chart review study (n = 67); in the prospective, single-arm, single-center, phase 2 TUXEDO‑1 study (n = 15); and in a retrospective cohort analysis of heavily pretreated patients with BMs (n = 10)23,24,25,26,27.
Here we report results from the phase 3b/4 DESTINY-Breast12 study (NCT04739761), a non-comparative study that evaluated the efficacy and safety of T-DXd in patients with HER2+ mBC from two separate cohorts of patients with and without baseline BMs. DESTINY-Breast12 is, to our knowledge, the largest prospective study of T-DXd in patients with HER2+ mBC with previously treated and stable or active (untreated or previously treated and progressing) BMs.
Results
Patients
A total of 504 patients were treated across 78 sites between June 2021 and February 2024; 263 patients had baseline BMs, and 241 patients had no baseline BMs (Fig. 1). Of patients with baseline BMs, 157 had previously treated and stable BMs, and 106 had active BMs (39 had untreated BMs; 67 had previously treated BMs that were progressive at study entry (hereafter termed previously treated/progressing BMs), with no clinical indication for immediate retreatment with local therapy). Demographics and baseline disease characteristics for both cohorts are summarized in Table 1. Patients with baseline BMs received a median of 1.0 regimen (range, 0–4) of previous anti-cancer therapy in the metastatic setting, and 158 patients (60.1%) received prior intracranial radiotherapy (including 40 patients (15.2%) who had WBRT and 15 (5.7%) who had SRS; the type of intracranial radiotherapy was not always recorded by investigators, and only WBRT and SRS intracranial radiotherapy were reported). Median time from last intracranial radiotherapy to treatment initiation in patients with prior intracranial radiotherapy was 164 d (range, 9–2,115) overall and 116.5 d (range, 9–1,798) and 214.5 d (range, 15–2,115) in the stable (n = 90) and active (n = 68) BMs subgroups, respectively. The median follow-up duration in this cohort was 15.4 months (range, 0.1–30.0), and 118 patients (44.9%) were continuing to receive treatment at final data cutoff (8 February 2024). The most common reasons for discontinuation of study treatment included progressive disease (PD; 30.8%) and adverse events (AEs; 11.8%) (Fig. 1). Patients with no baseline BMs received a median of 1.0 regimen (range, 0–4) of previous anti-cancer therapy in the metastatic setting and had a median follow-up duration of 16.1 months (range, 0.8–28.4); 95 patients (39.4%) were continuing to receive treatment at final data cutoff. Primary reasons for discontinuation of study treatment included PD (35.7%) and AEs (7.5%) (Fig. 1).
Response and progression in both cohorts were assessed by independent central review (ICR) per Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST 1.1).
Overall efficacy in the baseline BMs cohort
Overall PFS at 12 months was 61.6% (95% CI: 54.9–67.6) in all patients with BMs (Fig. 2a and Table 2) and 62.9% (95% CI: 54.0–70.5) and 59.6% (95% CI: 49.0–68.7) in patients with stable and active BMs, respectively (Table 2). Within the active BMs subgroup, PFS at 12 months was 47.0% (95% CI: 29.6–62.7) and 66.7% (95% CI: 53.4–76.9) in patients with untreated and previously treated/progressing BMs, respectively (post hoc analysis). Overall, 89 patients (33.8%) were free of progression at the time of the analysis, and median PFS (post hoc analysis) was 17.3 months (95% CI: 13.7–22.1). Time to progression (time from first dose until documented disease progression) data were immature, and the median was not calculated. Time to second progression (PFS2; time from first dose to second progression or death) data were immature, and the median was not reached. PFS2 at 12 months was 83.1% (95% CI: 77.5–87.4). Overall survival (OS) data were immature at the time of analysis (16.3% maturity); 12-month OS was 90.3% (95% CI: 85.9–93.4) (Fig. 2b and Table 2). In the baseline BMs full analysis set, confirmed ORR was 51.7% (95% CI: 45.7–57.8) (Table 2). A total of 11 patients (4.2%) had a complete response, and 125 (47.5%) patients had a partial response. Most responses (121/136) were reported by 6 months; at the time of analysis, response was ongoing in more than 50% of patients (n = 134 (51.0%)), and, therefore, median duration of response (DOR) was not calculated (Extended Data Fig. 1a). The ORR in patients with stable and active BMs was 49.7% (95% CI: 41.9–57.5) and 54.7% (95% CI: 45.2–64.2), respectively (Table 2). In a post hoc analysis restricted to patients with measurable disease at baseline (n = 198), confirmed ORR was 64.1% (95% CI: 57.5–70.8) overall and 67.0% (95% CI: 58.1–75.8) and 60.7% (95% CI: 50.5–70.8) in patients with stable (n = 109) and active (n = 89) BMs, respectively (Table 2). The best percentage change in target lesion size is shown in Fig. 3a….