Antibodies with specificity for one target — called monoclonal antibodies — were the first cancer immunotherapy to achieve widespread clinical use. The therapeutic potency of antibodies can be amplified by engineering them to recognize two distinct molecular targets (termed antigens). These bispecific antibodies can simultaneously bind to cancer cells and immune cells called T cells, and this dual binding directs the T cell to unleash its cell-killing power towards the cancer cell. Writing in Nature Cancer, Wu et al.1 now report the development of a trispecific antibody, one that has three targets: a cancer cell, a receptor that activates T cells, and a T-cell protein that promotes long-lasting T-cell activity against the cancer cell.
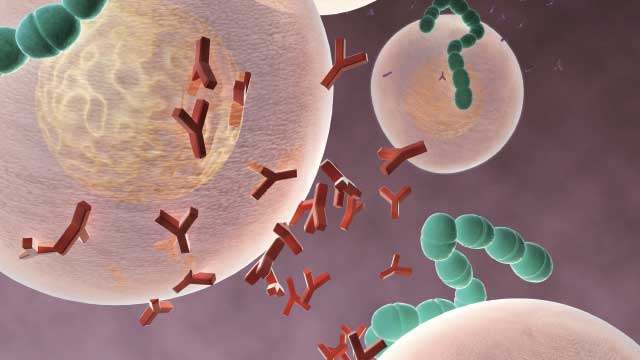
The mammalian immune system generates an immense diversity of antibodies, and antibodies can also be engineered to recognize therapeutic targets. Antibodies usually recognize a single antigen, which might be part of a disease-causing agent or an abnormal version of a protein or sugar. Such monospecific antibodies against targets on cancer cells can recruit immune cells, including neutrophils, natural killer cells and macrophages, to kill or ingest the cancer cells.
Antibodies can also be engineered to block or stimulate the function of the proteins to which they bind. For example, there are regulatory receptors that inhibit T-cell function, and antibodies that have been engineered to block these receptors provide a clinical strategy known as checkpoint blockade, which boosts T-cell function. These inhibitory receptors govern T-cell exhaustion, a non-functional T-cell state that protects against autoimmunity and that can occur in the tumour microenvironment as cancers evade antitumour responses mediated by T cells. Checkpoint-blockade treatment can awaken exhausted antitumour T cells to great clinical benefit, but it also risks causing autoimmune toxicity. The antibody developed by Wu and colleagues takes a similar approach to promote T-cell activity against cancer cells. However, their method stimulates the function of receptors that positively boost T-cell function, rather than blocking the function of inhibitory receptors.
The human antibody developed by Wu et al. builds on bispecific-antibody technology that reconfigures the antigen-recognition domains of two different antibodies into one bispecific molecule. Bispecific antibodies usually target one antigen on the cancer cell’s surface and one on a protein complex on T cells called CD3. CD3 is part of the T-cell receptor (TCR) complex. The TCR also includes antigen-recognition domains and delivers an activating signal to the T cell when an antigen binds. Engagement of CD3 by the antibody also generates an activating signal. Such a bispecific antibody therefore activates T cells, brings them into close proximity to cancer cells — irrespective of the T cell’s natural antigen specificity — and redirects their killing capabilities towards the cancer cells.
This concept has proved to be clinically effective for the bispecific antibody blinatumomab, which targets CD3 and the protein CD19 on cancer cells. Blinatumomab treatment doubles the remission rate and survival among people with an advanced stage of a cancer called B-cell acute lymphoblastic leukaemia (B-ALL)2, and it is being tested as part of the initial therapy for B-ALL, with promising early results3.
Wu and colleagues devised a clever strategy to simultaneously boost T-cell activation and enhance the targeting of cancer cells in relation to multiple myeloma, which is a cancer of plasma cells in the blood. The authors developed a trispecific antibody that was engineered to have three antigen-binding sites, rather than two. This trispecific antibody targets CD3 plus the proteins CD38 (on cancer cells) and CD28 (on T cells). The CD38-targeting antibody daratumumab is clinically effective in treating this disease4, and CD38 is also a potential target in other cancers, such as acute lymphoid leukaemia and acute myeloid leukaemia.
CD28 belongs to a class of protein called co-stimulatory receptors, which positively regulate T-cell activation. When a T cell recognizes its target antigen through the TCR, the extra engagement of a co-stimulatory receptor such as CD28 is needed to achieve the sustained T-cell proliferation required for an effective immune response. In the absence of co-stimulation, activation through the TCR can lead to a state of T-cell non-responsiveness called anergy, or to the related state of exhaustion. Prolonged activation of the TCR without co-stimulation can lead the T cell to undergo a form of programmed cell death called apoptosis.
The addition of a co-stimulatory signal such as CD28 is notable because this signal has also been incorporated into another type of immunotherapy called chimaeric-antigen receptor T cell (CAR‑T) therapy5, in which a receptor is engineered to both recognize a cancer-cell antigen and include T-cell activation domains such as CD3 and CD28. The main reason for including a CD28-binding domain in the trispecific antibody is T-cell co-stimulation. However, CD28 is also frequently expressed by multiple myeloma cells, so this might increase the antibody’s affinity for the myeloma cells, and thus enable it to bind to cells in which CD38 is low, absent or masked by previous daratumumab therapy….