A toxic anticancer therapeutic agent was encapsulated in capsules derived from apoferritin, which sequestered the drug until its selective delivery to cancer cells.
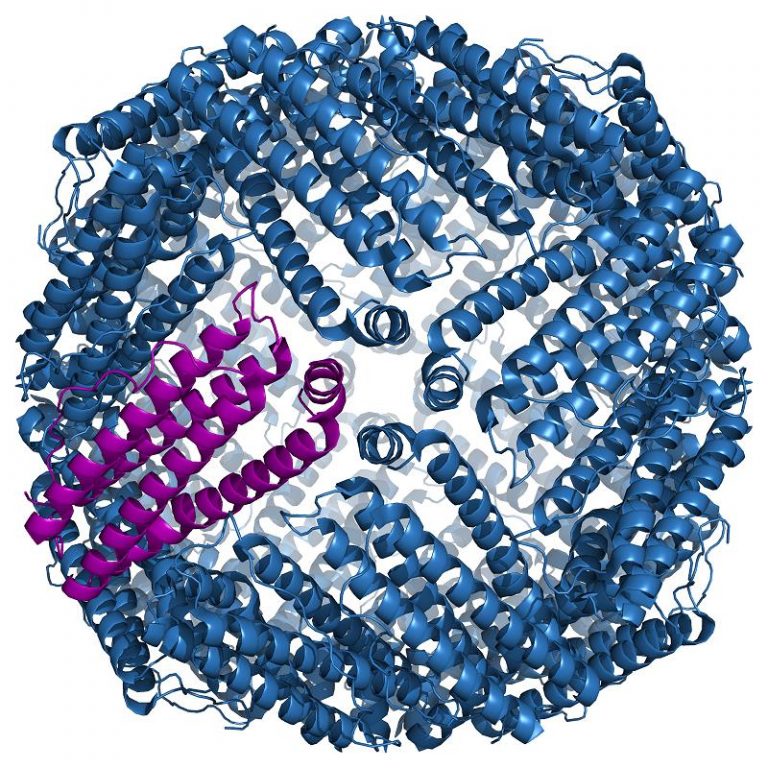
Ferritin is a globular protein complex consisting of 24 protein subunits and is the primary intracellular iron-storage protein in both prokaryotes and eukaryotes, keeping iron in a soluble and non-toxic form. Ferritin that is not combined with iron is called apoferritin.
Investigators at Washington State University (Pullman, USA) were looking for a better way to administer the anticancer drug daunorubicin. This drug interacts with DNA by intercalation and inhibition of macromolecular biosynthesis. This inhibits the progression of the enzyme topoisomerase II, which relaxes supercoils in DNA for transcription. Daunorubicin stabilizes the topoisomerase II complex after it has broken the DNA chain for replication, preventing the DNA double helix from being resealed and thereby stopping the process of replication. The drug is administered via rapid intravenous infusion. It cannot be given intramuscularly or subcutaneously, since it may cause extensive tissue necrosis. If administered into the spinal canal, it will cause extensive damage to the nervous system and may lead to death.
To circumvent daunorubicin’s toxic properties the investigators loaded a mixture of the hydrophobic drug and hydrophilic poly-L-aspartic acid (PLAA) into molecules of apoferritin under slightly acidic conditions that caused the apoferritin molecules to swell. Back at normal pH, the surface of the drug-carrying apoferritin capsules was modified with hyaluronic acid (HA), which targeted the capsules to the cancer cells’ to the HA-receptor CD44.
The drug-bearing capsules were used to treat cultures of human embryonic lung MRC-5 cells and lung cancer A549 cells. Results published in the October 2015 issue of the journal Biomaterials Science revealed that the drug was maintained within the capsules until delivery and subsequent uptake by the cancer cells. Release of the drug by the acidic environment of the cancer cells resulted in death of more than 70% of them with no damage to normal cells.
“Our efficiency in killing the cancer cell was very high with no toxicity to normal cells,” said senior author Dr. Yuehe Lin, professor of mechanical and materials engineering at Washington State University. “At the cell level, we were able to demonstrate it was very effective.”