There are a lot of unknowns when it comes to understanding how the mammalian respiratory tract responds to allergens, but a study published today (January 17) in Science Immunology, offers new insight. Researchers identified a group of epithelial cells in the mouse nose that are capable of responding to allergens directly and also to ATP released in response to allergens. When exposed to allergens, these so-called brush cells secrete cysteinyl leukotrienes, proinflammatory lipids that have been previously shown to come mostly from immune cells and have been linked to asthma and allergies.
“We have been interested in how allergens are recognized by the airway epithelium and how they drive immune responses that are biased towards allergic inflammation,” says coauthor Lora Bankova of Harvard Medical School.
Previous research had shown that tuft cells, a solitary chemosensory cell type found in the intestine, are responsible for orchestrating immunity to parasitic worms in the gut, which trigger the same type of immune response as allergens. To determine whether there might be cells playing the same role in the airway epithelium, she and her colleagues investigated a similar cell type in the mouse trachea: brush cells. In work published in 2018, they analyzed the gene expression profile of brush cells and found that brush cell activation was important for airway inflammation.
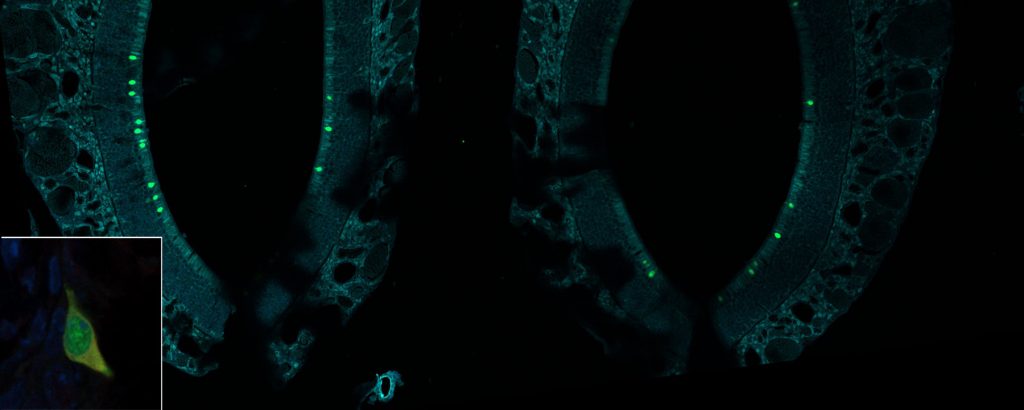
In the trachea, brush cells are only about half of a percent of the total number of cells. These small numbers made it hard to do in vitro or ex vivo cultures in which it would be possible to directly stimulate them and see what happens, Bankova explains. So the research team looked for these cells elsewhere in the airway. In the current study they found that there are solitary chemosensory cells with similar transcriptional profiles to the tracheal brush cells present in much larger numbers in the mouse nose, where they contribute 4–8 percent of the total cells.
“Because they’re so abundant we were actually able to isolate them and study them directly to see what activates them, what can they produce in response to stimulation,” Bankova tells The Scientist. The researchers isolated nasal brush cells from mice and incubated them with ATP, which functions as a cellular stress or damage signal, or with allergens from dust mites or mold.
In response, the brush cells released proinflammatory cysteinyl leukotrienes at amounts comparable to or exceeding what immune cells produced when the research team stimulated them. Brush cell production of these lipids, and the lower levels generated by other cell types, indicate that the epithelial cells are likely the dominant source of cysteinyl leukotrienes in the nose. The researchers also showed that mice without brush cells had a reduced amount of allergic inflammation in response to an allergen.
“Allergen activates them, and they’re important for generating the cysteinyl leukotrienes and allergic inflammation in that setting,” says Bankova. She explains that it’s likely that they’re also responding to other sorts of damage in the airway epithelium because they release cysteinyl leukotrienes in response to ATP as well.
That ATP serves as a ligand for brush cells is the most surprising finding, says Christoph Schneider, a biologist at the University of Zurich who did not participate in the study. He adds that open questions include whether or not brush cells are the sole target of ATP and sole source of cysteinyl leukotrienes and “whether this is true only for these airway brush cells or whether the same ATP effect is also observed in other situations, in other organs, et cetera.”
“To develop an asthma-like syndrome—especially if it’s allergic in nature—you have to have sensitization and then a subsequent response to challenge, so this is providing a mechanism by which the epithelium by itself is critical for sensitization,” says Teal Hallstrand, a pulmonary physician at the University of Washington who was not involved in the work. “I’d be very excited to learn about whether or not people with asthma have an alteration in the number of these cells in their airways and what specific physiological effect that has.”