After years of debate, the US Food and Drug Administration (FDA) is poised to allow the sale of biosimilars, cheaper versions of complex and expensive biological drugs used to treat conditions such as cancer and autoimmune diseases. On 7 January, an FDA advisory panel decided unanimously that a drug made by Sandoz, the generics arm of Swiss pharmaceutical giant Novartis, should be accepted as a replacement for filgrastim (Neupogen), an immune-boosting drug for people undergoing cancer treatment made by Amgen of Thousand Oaks, California.
Such knock-offs are called biosimilars because the drugs that they mimic, dubbed biologics, consist of complicated molecules that are made in living cells and are impossible to copy exactly. Even copying them inexactly is immensely challenging — despite the expected approval of the Sandoz drug, the difficulties involved in creating and evaluating biosimilars may limit their infiltration of the marketplace. The field is also littered with patent issues, especially with regard to how the drug is manufactured. In the case of filgrastim, Sandoz is challenging some of the legal requirements for approval.
“We’re starting from scratch,” says Jordan Paradise, a specialist in technology law at Seton Hall University in Newark, New Jersey. “A lot of the scientific uncertainty is still there.”
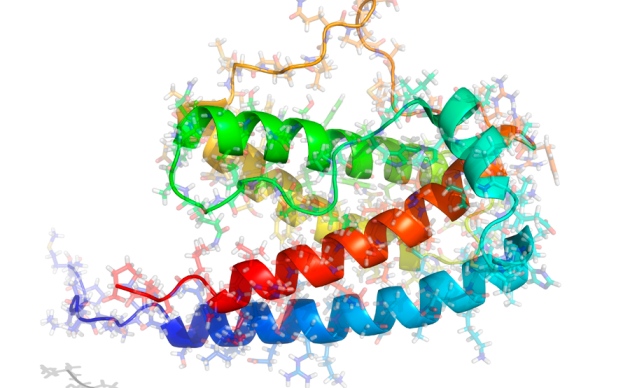
Unlike typical drugs, which are relatively small molecules made through biochemical processes, biologics are large protein molecules produced by genetically engineered organisms. Living cells may chemically modify the proteins they make by adding complex sugars and other compounds at certain positions. The exact conditions under which cells are grown can alter the pattern of these modifications, and thus the molecule’s structure and behaviour. The result is a drug so complex that it is difficult — if not impossible — to fully characterize.
Because biosimilars are inexact copies, they are required to undergo more testing than an ordinary generic drug. The European Union has been evaluating and approving biosimilars for the past decade, but the United States did not have a way to do so until regulatory legislation was passed in 2010. Biotechnology companies have been waiting to find out how the FDA would evaluate the drugs.
Patient advocates hope that biosimilars can reduce drug costs by increasing competition. Biologics are expensive: researchers have calculated that treatment of metastatic colorectal cancer with bevacizumab (Avastin) costs about US$75,000 per year of life gained (V. Shankaran et al. Oncologist 19, 892–899; 2014). A report last year by the RAND Corporation in Santa Monica, California, estimated that biosimilars could save $44.2 billion by 2024.
Filgrastim is relatively simple: it is a small protein with no attached sugars. Even so, Sandoz presented the FDA with clinical-trial data from 388 people with breast cancer and 174 healthy participants to show that its biosimilar breaks down in the body similarly to the original, and does not provoke an immune response.
The FDA is expected to make a final decision by May. But even as Sandoz prepares to sell its drug in the United States, it is embroiled in a patent fight with Amgen. By US law, Sandoz had to reveal the details of its manufacturing method to Amgen — a provision not present in Europe — so that Amgen could determine whether any of its patents had been violated. Sandoz refused. That is a disheartening precedent, says Paradise. “Here we’ve got the first biosimilar application and we’ve already got the manufacturers not working together.”
Such concerns loom large among manufacturers, says Nicholson Price, a patent-law specialist at the University of New Hampshire School of Law in Concord. Drug firms often keep their manufacturing methods confidential, and production of complex drugs gives them ample opportunity to file patents on manufacturing techniques or ways of characterizing molecules. “The second company is attempting to feel its way in the dark to what the first company has done,” says Price. “I suspect there are other biosimilars that are being deterred either by specific patents or just the worry that there may be patents lurking out there that they don’t know about.”
Even when a biosimilar makes it over these hurdles, it is unclear how consumers will react to a drug that is almost, but not quite, a copy of the original. At the advisory-committee meeting, a number of patient groups expressed support for biosimilars and the promise of relief from high drug prices. But they voiced concerns that biosimilars would be given the same generic names as the drugs they were meant to replace, creating confusion as to whether recipients were getting the original or the copy. Many will be watching the Sandoz drug’s approval to see whether the FDA will let it be called filgrastim.
Committee member James Liebmann, an oncologist at the University of Massachusetts in Worcester, reacted to that concern with surprise. “This has been pretty clearly shown to be filgrastim,” he said. “To name it anything else would be misleading.”