Instructing the immune system to recognize and kill tumours, an approach termed cancer immunotherapy, has transformed the clinical treatment of certain types of malignancy. Prominent among these therapies are immune-checkpoint inhibitors, which block the action of proteins that dampen immune-cell responses against tumours. For example, antibodies can be used to interfere with the inhibitory protein PD-1, which is present on T cells, a type of immune cell that attacks tumours. Immune-checkpoint inhibitors have been most successfully used to treat cancers, such as melanomas, that are well infiltrated by T cells and have a large number of genetic mutations1,2. A subset of these mutations might generate neoantigens — altered protein sequences that are uniquely produced in cancer cells and are recognized as foreign by the immune system.
Read the paper: Actively personalized vaccination trial for newly diagnosed glioblastoma
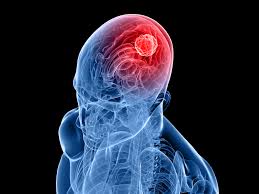
Most cancers, however, including brain tumours called glioblastomas, do not respond to immune-checkpoint therapy. These non-responsive tumours typically have a low level of mutations and express few neoantigens; that is, they have an immunosuppressively ‘cold’ tumour microenvironment . They therefore fail to attract T cells that can infiltrate the tumour. Finding ways to boost an immune response to such tumours is an ongoing challenge. Writing in Nature, Keskin et al.4 and Hilf et al.5 report their progress in this area, and present the results of separate phase I clinical trials in which people with glioblastoma were treated with a personalized vaccine containing neoantigens that were specific to the individual’s own tumour….