Selective delivery of copper (Cu) to the central nervous system effectively treats the motor neuron disease amyotrophic lateral sclerosis (ALS) in the most widely used mouse model of the disorder.
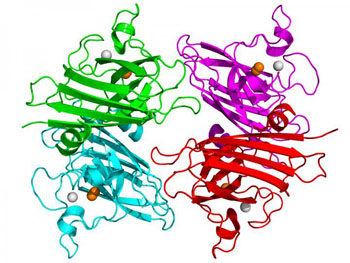
ALS is a progressive and fatal neurodegenerative disease caused by the death and deterioration of motor neurons in the spinal cord that is linked to mutations in the enzyme copper, zinc superoxide dismutase (Cu, Zn SOD). Copper helps to stabilize the three-dimensional structure of this antioxidant enzyme, but when it lacks metal co-factors, SOD can unfold and become toxic, leading to the death of motor neurons.
Over-expression of mutant Cu, Zn SOD in mice induces ALS and has become the most widely used model of neurodegeneration. However, no pharmaceutical agent in 20 years has extended lifespan of these animals by more than a few weeks.
The Copper-Chaperone-for-SOD (CCS) protein completes the maturation of SOD by inserting copper, but paradoxically mice that have been genetically engineered to express human CCS while co-expressing mutant SOD die within two weeks of birth.
Hypothesizing that co-expression of CCS created copper deficiency in the spinal cord, investigators at Oregon State University (Corvallis, USA) treated these baby mice with the PET (positron emission tomography)-imaging agent CuATSM (diacetyl-bis(N4-methylthiosemicarbazone)), which is known to deliver copper into the central nervous system within minutes.
The investigators reported in the January 27, 2016, online edition of the journal Neurobiology of Disease that CuATSM prevented the early mortality of the CCSxSOD mice, while markedly increasing the level of Cu, Zn SOD protein in their ventral spinal cords. Remarkably, continued treatment with CuATSM extended the survival of these mice by an average of 18 months. When CuATSM treatment was stopped, these mice developed ALS-related symptoms and died within three months. Restoring CuATSM treatment could rescue these mice after they became symptomatic, providing a means to start and stop disease progression.
All human ALS patients express CCS, raising the hope that familial ALS patients could respond to CuATSM treatment similarly to the CCSxSOD mice.
“We are shocked at how well this treatment can stop the progression of ALS,” said senior author Dr. Joseph Beckman, professor of biochemistry and at Oregon State University. “We have a solid understanding of why the treatment works in the mice, and we predict it should work in both familial and possibly sporadic human patients, but we will not know until we try. We want people to understand that we are moving to human trials as quickly as we can. In humans who develop ALS, the average time from onset to death is only three to four years.”