Infection with the SARS-CoV-2 virus can lead to diverse outcomes, ranging from no symptoms to varying degrees of disease severity, spanning mild illness to death. What determines the degree of severity is unclear, but mounting evidence points to exacerbated and abnormal responses in the innate branch of the immune system as a main driver of major illness. Writing in Nature, Combes et al.1 present a study investigating the hallmarks of COVID-19 severity.
The authors analysed cells, including immune cells, in blood samples from 21 people with COVID-19 and 25 uninfected individuals who were either healthy or had a lung injury or breathing difficulties. They monitored gene expression during the course of the infection as patients went on to develop either what was categorized as mild–moderate COVID-19 (which required a short hospital stay without the need for intensive care or mechanical ventilation) or severe COVID-19 (requiring intensive care and mechanical ventilation). The authors found that the cells of people with mild–moderate COVID-19 expressed a distinct set of genes whose expression depends on what are known as type I interferon proteins. Interferons, molecules that are also called cytokines, drive the expression of genes that have a role in antiviral defence.
This interferon-regulated gene-expression signature was not observed in the cells of people with severe COVID-19. Instead, the cells had a gene-expression signature described as an inflammatory S100A12 myeloid-cell program (S100A12 is a protein expressed as part of this program). A S100A12 signature was previously identified2 as being associated with severe COVID-19. Interestingly, a similar program is associated with another form of severe disease called sepsis, which derives from an aberrant immune response to bacterial infection3.
An interferon-regulated gene-expression program can be crucial to defence against viral infection, so the lack of activation of this program in people with severe COVID-19 provided a hint that defective initiation of this pathway might contribute to the observed differences in disease severity. Combes et al. therefore set out to determine the reason for the differences. The first obvious suspect was the level of an interferon protein (IFN-α) in blood plasma (blood lacking its cellular content). The authors found no notable difference in IFN-α levels with differing disease severity. However, there are other types of interferon protein that the authors did not measure.
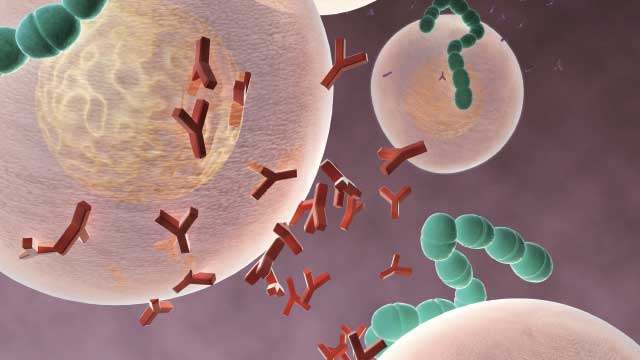
The authors next turned their attention to antibodies. Antibodies against SARS-CoV-2 have a protective role in the natural immune response to this virus, and antibodies targeting the virus have been used as COVID-19 treatments. Indeed, part of the rationale for using the vaccines currently available is to drive the generation of such antibodies. The authors found that the level of antibodies against the SARS-CoV-2 spike and nucleocapsid proteins was higher in people with severe disease than in those with mild–moderate COVID-19. Moreover, high antibody levels were negatively correlated with the presence of cells expressing an interferon-regulated gene-expression program.