In 2010, 5-year-old Emily Whitehead was diagnosed with acute lymphoblastic leukemia (ALL). Though her parents were told that if you had to have a kid with cancer, ALL was the best one to have, Emily’s course was hardly typical. After two rounds of chemotherapy, necrotizing fasciitis developed in both legs and she barely avoided amputation. Sixteen months later, she had a relapse. Bone marrow transplantation was recommended, but the Whiteheads, concerned about toxic effects, sought a second opinion at Children’s Hospital of Pennsylvania. There they learned about a new therapy, developed by University of Pennsylvania investigators and known as CART-19, which involved genetically engineering the patient’s own T cells to kill tumor cells.
Unfortunately, a clinical trial had not yet been cleared by the Food and Drug Administration (FDA), and Emily’s leukemic cells were doubling daily. So Emily returned to her local hospital and received another round of intensive chemotherapy, which bought her 3 weeks but no remission. Out of options, one oncologist recommended hospice. But “That just didn’t make sense to us,” says Tom Whitehead, Emily’s father. When the Whiteheads said they wanted to return to Children’s Hospital, the oncologist told them that hospice was preferable to entering Emily into an experimental study that wouldn’t help her get better.
But her parents opted to enroll her in a study, and she became the first child to receive CART-19. As a result, not only is she now a thriving 12-year-old, but her survival helped reenergize a line of research that was nearing failure. In August 2017, the FDA approved the first chimeric antigen receptor T-cell (CAR-T) therapy, Novartis’s tisagenlecleucel, which uses the Penn-developed technology, for patients up to 25 years of age with relapsed or refractory ALL. Though the indication is narrow, the results are striking in a patient population with otherwise limited options: 83% of the 63 evaluable children who received tisagenlecleucel in Novartis’s phase 2 trial had complete elimination of malignant cells at 3 months.1
The approval is probably the first of many for CAR-T products. Gilead recently announced its $11.9 billion acquisition of Kite Pharma, whose CAR-T technology, initially developed at the National Institutes of Health (NIH), has shown efficacy in patients with chemorefractory, aggressive B-cell non-Hodgkin’s lymphoma.2 And some 40 other companies, many in partnership with academic institutions, are racing to develop CAR-T technologies for myriad indications. Though early data are most promising for other hematologic cancers, such as relapsed chronic lymphocytic leukemia (CLL),3 similar therapies may eventually prove effective for solid tumors as well.
The emergence of CAR-T therapy, like most scientific advances, reflects the incremental insights of hundreds of scientists over decades — from surgeon William Coley’s recognition of the immune system’s potential for treating cancer when, in 1893, he injected streptococcus into inoperable osteosarcoma and observed the tumor shrink, to the making of the first CAR-T cells by the Israeli immunologist Zelig Eshhar in 1993.4 Indeed, the story of CAR-T therapy says as much about the methodical nature of scientific progress as it does about the passions that sustain it.
As Carl June, the immunologist who led the development of Penn’s CAR-T technology, recalled, “So many times, I almost had to quit.” June spent his early career developing a technique to boost immune function in patients with HIV by modifying their T cells and inducing proliferation ex vivo. Though he and his colleague Bruce Levine would later build on this technique to engineer patients’ T cells to attack leukemia, June might have continued focusing solely on the basic science. But in 1996, his 41-year-old wife was diagnosed with ovarian cancer. June tried unsuccessfully to get a pharmaceutical company to provide the tools he needed to attempt immunotherapy. When his wife died in 2001, June resolved to apply emerging immunologic insights to the development of cancer therapies, even though that meant creating a biotech infrastructure within academia.
The translational hurdles remained formidable. The field had been dogged by skepticism and setbacks, and the NIH wouldn’t fund a clinical trial. Once again, tragedy propelled the research forward. In 2001, Barbara and Edward Netter, having watched their daughter-in-law die of breast cancer, started the Alliance for Cancer Gene Therapy (ACGT), hoping to develop alternative approaches. In 2008, ACGT granted June and his coinvestigator David Porter $1 million, enough to treat their first three patients with relapsed CLL with CART-19. Two of the three patients achieved complete remission, but the investigators ran out of funding. Knowing they couldn’t prove efficacy statistically, they published their findings as case reports.3,5 Soon, the National Cancer Institute offered June a grant, and Novartis licensed Penn’s CAR-T technology. But June acknowledges the tenuous nature of anecdote: “Were we lucky? Were they representative? Would it be durable?”
Indeed, anecdote can easily break a field rather than make it: the death of Jesse Gelsinger in a trial at Penn had set the field of gene therapy back at least a decade. And as both June and Stephan Grupp, the Children’s Hospital oncologist and principal investigator of the CART-19 trial in children, emphasized, had Emily died, the CAR-T field would probably have died with her. But though unexpected toxic effects in phase 1 studies can fell any new therapy, the unfortunate reality is that it often takes time, and human lives, to distinguish fatal toxic effects from those that can be managed. As Grupp explained, “There was no way to predict a great deal of what we learned. The toxicity issues can only be learned from human beings.”
Emily Whitehead was a case in point. After receiving her third dose of CART-19, she developed high fevers, respiratory failure, and shock necessitating the use of three pressors. Though Emily was experiencing what’s now understood to be cytokine-release syndrome, which occurred in 78% of patients in Novartis’s phase 2 trial, it wasn’t clear at the time what was driving this response, much less how to treat it.
That she survived gives new meaning to the adage “Chance favors the prepared mind.” Per protocol, participants’ blood was sent for cytokine analysis, with about a 2-week turnaround time. But as Emily rapidly deteriorated, Grupp called the lab and begged them to run Emily’s blood more quickly. Two hours later, in time for his 3 p.m. lab meeting, Grupp learned that Emily’s level of interleukin-6 was elevated 1000-fold. He recalls the meeting, as everyone pored over the results. “No one thought we should be thinking about this thing, IL6,” Grupp explained. “It isn’t even made by T cells.” That fact, however, made interleukin-6 acceptable for Emily’s doctors to target, since any interference with T-cell function could interfere with the antileukemic activity, without which she would die. But how to quash interleukin-6? As Grupp and his lab members started Googling, June, giving a talk in Seattle, received the results and had an idea. His daughter, who has juvenile rheumatoid arthritis, had recently started taking tocilizumab, a monoclonal antibody that targets interleukin-6. As the investigators converged on a similar conclusion, one hurdle remained: how to get the drug in time for Emily?
Once again, they got lucky. Tocilizumab was on the hospital’s formulary for rheumatologic indications, which meant that rather than having to wait for up to 2 days, by 8 p.m. that evening, Emily received a dose. Within hours, she began to improve, so dramatically that her doctors could barely wean the pressors fast enough. On her seventh birthday, Emily woke up. Eight days later, on the basis of a bone marrow biopsy, Grupp reported that the treatment had worked.
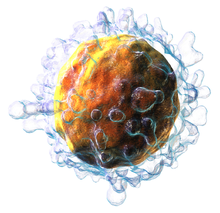
Though the remissions achieved with CAR-T therapy are impressive, much remains unknown. CAR-T products vary in ways that will have implications for both efficacy and toxicity. Some variation arises from the chimeric antigen receptors (CARs) themselves, which are programmed to recognize various antigens and contain various types and numbers of costimulatory domains to induce proliferation. In the case of CART-19, for instance, the engineered T cells bind to lymphocytes displaying the CD19 antigen, a hallmark of leukemic B cells and thus an attractive target because humans can tolerate B-cell aplasia. Identifying antigen targets in solid tumors while preventing destruction of healthy tissue remains challenging, however, especially since the tumor microenvironment can be immunologically hostile to introduction of a CAR. Moreover, toxicities remain formidable. Though tocilizumab is now often used to manage the cytokine-release syndrome, other toxic effects, such as cerebral edema, remain poorly understood and difficult to manage.
Meanwhile, the CAR-T discussion has become dominated by cost concerns. Critics argue that tisagenlecleucel’s $475,000 price tag is unaffordable and unjustifiable given the taxpayer-supported basic research underpinning its development, while manufacturers point to the tremendous investment required to produce the drug and fund trials. With many patients unable to afford their medications and ongoing instances of unconscionable drug-company profiteering, these discussions are both essential and complex. Regardless of the finances, we all hope that these remissions are prolonged or, even better, turn out to be cures. There is no way to know whether they will without prolonged observation, but while we carefully observe each patient, it is important to remember that therapeutic advances are motivated by more than money — that it’s the hope, vision, and perseverance of both patients and investigators that have made this critical conversation possible.